Professional Documents
Culture Documents
Patho Ards
Uploaded by
Johanisa SultanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Patho Ards
Uploaded by
Johanisa SultanCopyright:
Available Formats
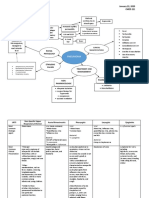
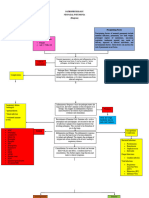
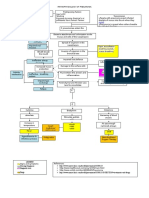
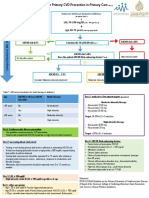
LEGEND:
Pathophysiology
ACUTE RESPIRATORY DISTRESS SYNDROME (ARDS)
Mechanism PATHOPHYSIOLOGY
Phases of ARDS DIRECT LUNG INJURY INDIRECT LUNG INJURY
•Pneumonia • Sepsis
Complications • Lung Trauma (Pulmonary Contusion) • Pancreatitis
• Near Drowning Foreign organisms or chemicals enters the alveoli • Fat Emboli
Signs and symptoms • Chemical pneumonitis from aspiration or
c • Transfusion-related acute lung injury (TRALI)
direct inhalation • Drug overdose
Diagnostic and laboratory findings
Damage the type 1 and type 2 pneumocytes
Management
Activation of immune system. Macrophages act as sentinels for the lungs
Pneumocytes secrete inflammataory cytokines e.g. TNF, IL-1, IL-6, & IL-8
Diffuse damage to the capillary endothelium and alveolar endothelium
After 24 hours of injury Neutrophils leaks into the Presence of cytokines in the site Toxic mediators cause ↑ permeability
further damage to the Fluid leaks Inflammation Fluid wash Dysfunction of
interstitium and enters stimulates the neutrophils to of alveolar Alveolar
type 1 and type 2 in the of alveoli away surfactant
the alveoli secrete toxic mediators e.g. endothelium collapse
pneumocytes alveoli surfactant
reactive O2 species and proteases
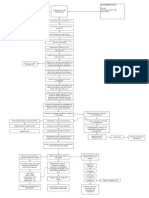
EXUDATIVE IL- 8 stimulates V/Q mismatch
PHASE neutrophil recruitment
Hypoxia
Damaged epithelium impairs gas exchange Hypoxemia
Neutrophil infiltration and Dyspnea
proinflammatory cytokines Tachycardia
Pulmonary capillaries do not adequately Pulmonary edema Tachypnea
lead to tissue edema,
dysfunction, and absorb fluid Cyanosis
subsequent destruction of
pulmonary epithelium Deposition of hyaline membranes in the ↓ elasticity in the ↓compliance of
Body attempts to heal lung tissue Impaired gas diffusion
alveoli alveoli the alveoli
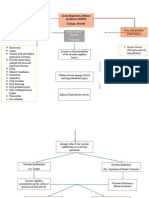
After 14 days of
injury
Supply the healing
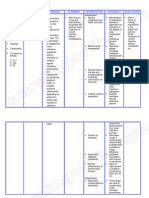
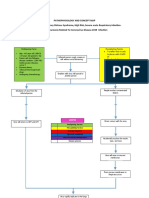
tissue with NURSING MANAGEMENT:
Hypoxia triggers Formulation of new nutrients and •Assess breath sounds (determine
angiogenesis blood vessels oxygen presence of crackles or rales sound).
•Monitor O2 saturation and symptoms.
PROLIFERATIVE •Monitor respiration and depth of
PHASE Type II alveolar Regenerates ↑PaO2
Differentiates to Repaired lung respiration.
epithelial cell damaged Eupnea ↓PaCO2
type I alveolar tissue •Assess ABG level.
proliferation epithelium ↓O2 requirement
cells •Assess Pt mental status.
Clearing of CXR
•Monitor blood chemistry and fluid levels.
•Assess chest x-ray.
Activation of Production of •Assist pt in a prone position optimizes
fibroblasts collagen and other Collagen deposition respiration.
ECM components •Prepare the client for intubation as
indicated.
•Monitor ventilation alarms and settings.
•For pt prognosed to fibrotic ARDS: Long
term O2supplementation/ventilation.
If it is not successful, •Manage Nutrition.
the tissue transition
to the fibrotic phase
MEDICAL MANAGEMENT:
•No definitive pharmacology
Unresolved infection, ↑PaCO2 treatments
Chronic Activation of Formulation Tissue re- Impaired ↓PaO2
prolonged mechanical •Supportive care: Oxygen therapy
inflammation fibroblasts of scar tissue modelling organ ↓SpO2
ventilation, or continuous •Extracorporeal technique (ECMO)
and function Bilateral opacity of CXR
exposure to irritants •Adjunctive pharmacologic
disruption
treatment:
Neuromuscular blockade
Corticosteroids
FIBROTIC Dyspnea Pulmonary vasodilators
PHASE Distortion and Persistent cough Anti-inflammatory agents
thickening of the Nail clubbing Beta agonists
Excessive accumulation of ↑ resistance in the Pulmonary
alveolar walls, Fatigue
collagen and other ECM pulmonary circulation hypertension
narrowing of the Chest pain
proteins in the lung tissue
airways, and the
formation of fibrous SURGICAL MANAGEMENT:
bands Surgical Lung Biopsy (to diagnose pulmonary
Right sided heart fibrosis).
failure Extracorporeal membrane oxygenation (ECMO).
Lung Transplantation
You might also like
- Pathophysiology Sa CobidDocument7 pagesPathophysiology Sa Cobidkuro hanabusa100% (2)
- Meyler's Side Effects of Drugs Used in AnesthesiaFrom EverandMeyler's Side Effects of Drugs Used in AnesthesiaRating: 5 out of 5 stars5/5 (2)
- Lecture 3 NeuropsychoanalysisDocument31 pagesLecture 3 NeuropsychoanalysisjobinNo ratings yet
- Pathophysiology: Patient B's Age: 28 Years OldDocument7 pagesPathophysiology: Patient B's Age: 28 Years Oldkuro hanabusaNo ratings yet
- 5drug StudyDocument7 pages5drug StudyPALEN, DONNA GRACE B.No ratings yet
- MANATAD, Dione Kirk D. January 22, 2020 MD-2035638 CMED 221 Concept Map: PneumoniaDocument4 pagesMANATAD, Dione Kirk D. January 22, 2020 MD-2035638 CMED 221 Concept Map: PneumoniaDK ManatadNo ratings yet
- LIGHT Pneumonia Dr. ConstantinoDocument6 pagesLIGHT Pneumonia Dr. ConstantinoMiguel Cuevas DolotNo ratings yet
- Patient Based PathophysiologyDocument3 pagesPatient Based PathophysiologyJeizel IgnacioNo ratings yet
- Pneumococcal PneumoniaDocument1 pagePneumococcal PneumoniaKierzteen Brianna TaromaNo ratings yet
- Covid and Ebola MsDocument7 pagesCovid and Ebola MsAimee Rochelle MaesaNo ratings yet
- Pathophysiology of Septic Shock Draft 1Document1 pagePathophysiology of Septic Shock Draft 1Ju Lie AnnNo ratings yet
- Pcap C Case StudyDocument21 pagesPcap C Case StudyKate PedzNo ratings yet
- Pcap PathophysiologyDocument3 pagesPcap PathophysiologyZandra Lyn AlundayNo ratings yet
- 3-Upper Respiratory DisordersDocument27 pages3-Upper Respiratory DisordersEllyza EvangelistaNo ratings yet
- Lower Respiratory Tract Infection (Pneumonia)Document4 pagesLower Respiratory Tract Infection (Pneumonia)krvpriya0No ratings yet
- Nursing Care Plan Neonatal PneumoniaDocument2 pagesNursing Care Plan Neonatal Pneumoniaderic93% (42)
- Pathophysiology Plueral Effusion Secondary To Pneumonia: GreenDocument7 pagesPathophysiology Plueral Effusion Secondary To Pneumonia: Greenkuro hanabusaNo ratings yet
- Dr. Constatntino: PneumomiaDocument4 pagesDr. Constatntino: PneumomiaAnn Ross VidalNo ratings yet
- Abas, Pathophysiology of CapDocument1 pageAbas, Pathophysiology of Capalexander abasNo ratings yet
- Infectious Disorder: Prepared By: Dellero, Sarah Joy P. BSN3-DDocument19 pagesInfectious Disorder: Prepared By: Dellero, Sarah Joy P. BSN3-Dngoto88No ratings yet
- Predisposing Factors Disease Precipitating Factors: LegendDocument3 pagesPredisposing Factors Disease Precipitating Factors: LegendSOPHIA LOISE TEJANO FULACHENo ratings yet
- Concept Map SampleDocument1 pageConcept Map SampleJet MaravillaNo ratings yet
- 6 CapDocument24 pages6 CapAyush GodhaniNo ratings yet
- Lung Scintigraphy in Various Lung PathologiesDocument50 pagesLung Scintigraphy in Various Lung PathologiesAnonymous RqEtRdNo ratings yet
- Neonatal Pneumonia Pathophysiology - FINALDocument5 pagesNeonatal Pneumonia Pathophysiology - FINALRoderick EstrellaNo ratings yet
- Microbiology 19 PDFDocument6 pagesMicrobiology 19 PDFLyka Villagracia AsiloNo ratings yet
- Pneumonie Interstitiala Articol EnglezaDocument57 pagesPneumonie Interstitiala Articol EnglezaRoxana PascalNo ratings yet
- ICC AUDIT TOOL AND TRIAGE ALGORHYTHM DGMC - WPS PDF Convert PDFDocument40 pagesICC AUDIT TOOL AND TRIAGE ALGORHYTHM DGMC - WPS PDF Convert PDFWendy Dela PenaNo ratings yet
- Pneumonia: TranscribersDocument6 pagesPneumonia: TranscribersIsabel CastilloNo ratings yet
- Pioquinto (Rot 2 Drug Study)Document8 pagesPioquinto (Rot 2 Drug Study)Ghianx Carlox PioquintoxNo ratings yet
- Neonatal Pneumonia PathophysiologyDocument5 pagesNeonatal Pneumonia PathophysiologyRoderick EstrellaNo ratings yet
- Pathophysiology of PneumoniaDocument2 pagesPathophysiology of PneumoniaAzria John DemetriNo ratings yet
- QCHDDocument1 pageQCHDmidskiescreamzNo ratings yet
- Lung CancerDocument23 pagesLung CancerCristel Gervacio SumayanNo ratings yet
- Antifungal and Antiparasitics AgentsDocument38 pagesAntifungal and Antiparasitics AgentsabdeljelileNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanJehan Lois QuinesNo ratings yet
- Pathology Lecture 1 MSADocument6 pagesPathology Lecture 1 MSAcejix87209No ratings yet
- Oral Revalida FinalsDocument10 pagesOral Revalida FinalsRaven PerejaNo ratings yet
- Pcap Pathophysiology PDFDocument3 pagesPcap Pathophysiology PDFMikaela RamosNo ratings yet
- Acute Respiratory Distress Syndrome - PathophysiologyDocument5 pagesAcute Respiratory Distress Syndrome - PathophysiologyJoann67% (3)
- Community Acquired Pneumonia Concept MapDocument1 pageCommunity Acquired Pneumonia Concept MapSebastianNo ratings yet
- Activity 2 Critical ThinkingDocument3 pagesActivity 2 Critical ThinkingWILJOHN DE LA CRUZNo ratings yet
- NCM112 LP2 TransesDocument9 pagesNCM112 LP2 TransesChristine CalleyNo ratings yet
- Non-Modifiable Risk Factor Modifiable Risk Factors: Acute Respiratory Distress Syndrome (ARDS) (Lungs Alveoli)Document3 pagesNon-Modifiable Risk Factor Modifiable Risk Factors: Acute Respiratory Distress Syndrome (ARDS) (Lungs Alveoli)joyrena ochondraNo ratings yet
- Concept Map CovidDocument7 pagesConcept Map CovidMaieca Demecillo100% (3)
- Case Study 4 CVD Infarct CAP MR HUD RDU DementiaDocument21 pagesCase Study 4 CVD Infarct CAP MR HUD RDU DementiaVictoria Mae Irong CabahugNo ratings yet
- PathDocument1 pagePathChristian Angelo LeonorNo ratings yet
- Pathophysiology of PneumoniaDocument2 pagesPathophysiology of PneumoniaJesselle LasernaNo ratings yet
- CNS+Infection+ +Fatima+SeparaDocument20 pagesCNS+Infection+ +Fatima+SeparaMarc Lorenz SeparaNo ratings yet
- 7.chest and Lower Respiratory Tract DisordersDocument8 pages7.chest and Lower Respiratory Tract Disorders2BGrp3Plaza, Anna MaeNo ratings yet
- My Co PlasmaDocument2 pagesMy Co PlasmaSravanthi UKNo ratings yet
- Minocycline One - Pager PDFDocument2 pagesMinocycline One - Pager PDFInês GouveiaNo ratings yet
- Pathophysiology of PneumoniaDocument2 pagesPathophysiology of PneumoniaJeffrey Ramos100% (1)
- The Complications of Tracheal Intubation A New.5Document12 pagesThe Complications of Tracheal Intubation A New.5osondoarNo ratings yet
- Advances in Metabolic Disorders: Volume 3From EverandAdvances in Metabolic Disorders: Volume 3Rachmiel LevineNo ratings yet
- Human Tumours Secreting Catecholamines: Clinical and Physiopathological Study of the PheochromocytomasFrom EverandHuman Tumours Secreting Catecholamines: Clinical and Physiopathological Study of the PheochromocytomasRating: 5 out of 5 stars5/5 (1)
- Pulmonary Infection in the Immunocompromised Patient: Strategies for ManagementFrom EverandPulmonary Infection in the Immunocompromised Patient: Strategies for ManagementCarlos AgustiNo ratings yet
- Opd ProceduresDocument4 pagesOpd ProceduresJohanisa SultanNo ratings yet
- Chapter IDocument8 pagesChapter IJohanisa SultanNo ratings yet
- Sultan - NCP 1 (Preterm Labor)Document2 pagesSultan - NCP 1 (Preterm Labor)Johanisa SultanNo ratings yet
- #3 Ass NSG126Document1 page#3 Ass NSG126Johanisa SultanNo ratings yet
- UntitledDocument1 pageUntitledJohanisa SultanNo ratings yet
- A Study of The Effects of Pet Ownership On Mental Health Among CoDocument107 pagesA Study of The Effects of Pet Ownership On Mental Health Among CoJohanisa SultanNo ratings yet
- UntitledDocument17 pagesUntitledJohanisa SultanNo ratings yet
- NCP2 (Sultan, J.) - Chronic Kidney DiseaseDocument2 pagesNCP2 (Sultan, J.) - Chronic Kidney DiseaseJohanisa SultanNo ratings yet
- E. Nursing Management (Highlight The Priority Nursing Interventions)Document6 pagesE. Nursing Management (Highlight The Priority Nursing Interventions)Johanisa SultanNo ratings yet
- UntitledDocument3 pagesUntitledJohanisa SultanNo ratings yet
- Coordination of Benefits QuestionnaireDocument2 pagesCoordination of Benefits Questionnairesamual prakashNo ratings yet
- Hindmarsh Analysis of Pandemic V.22.11.2021aDocument97 pagesHindmarsh Analysis of Pandemic V.22.11.2021autopikNo ratings yet
- Dyslipidemia Final Poster June 24Document2 pagesDyslipidemia Final Poster June 24drabdulrabbNo ratings yet
- Insulin and Oral Hypoglycemic DrugsDocument45 pagesInsulin and Oral Hypoglycemic DrugsRamadi PrameelaNo ratings yet
- Keissa Davis Operating Room ExperienceDocument2 pagesKeissa Davis Operating Room ExperiencePatricia Marie Laman YadaoNo ratings yet
- Concept Essay IdeasDocument10 pagesConcept Essay Ideasd3gpmvqw100% (2)
- Dialogue On Saudi National DayDocument2 pagesDialogue On Saudi National DayZainabNo ratings yet
- Download pdf Case Studies In Veterinary Immunology 1St Edition Laurel Gershwin Author ebook full chapterDocument53 pagesDownload pdf Case Studies In Veterinary Immunology 1St Edition Laurel Gershwin Author ebook full chapterjaime.currie230100% (2)
- Clinical Exam of The Psychiatric PX HX MSE Signs Symptoms Modified For Senior Clerks 2021Document139 pagesClinical Exam of The Psychiatric PX HX MSE Signs Symptoms Modified For Senior Clerks 2021Rakesh KumarNo ratings yet
- Mapeh 5 - Dominican School: Achieving Excellence TogetherDocument5 pagesMapeh 5 - Dominican School: Achieving Excellence TogetherLilian VergaraNo ratings yet
- DIY HRT Harm Reduction Guide PDFDocument11 pagesDIY HRT Harm Reduction Guide PDFKentucky Trans Health JusticeNo ratings yet
- Cancer ImmunologyDocument31 pagesCancer ImmunologyAbdul FarooqNo ratings yet
- Full Download Daviss Drug Guide For Nurses 16th Edition Vallerand Test BankDocument32 pagesFull Download Daviss Drug Guide For Nurses 16th Edition Vallerand Test Bankjaydejakabfx100% (32)
- 6 - Original Article PDFDocument7 pages6 - Original Article PDFIna BogdanNo ratings yet
- Anat&Physio Test Cherrie Lan SSSS16 PDFDocument14 pagesAnat&Physio Test Cherrie Lan SSSS16 PDFPriyanka singhNo ratings yet
- 500 Series SMAW MG Msds 8-06Document3 pages500 Series SMAW MG Msds 8-06mohamed AdelNo ratings yet
- Body Fat Estimate (US Navy Formula) Calculator FormulasDocument1 pageBody Fat Estimate (US Navy Formula) Calculator FormulasSantiago MedinaNo ratings yet
- Increase Height and Grow Taller Using Brain Wave Binaural Beats - Natural Height GrowthDocument12 pagesIncrease Height and Grow Taller Using Brain Wave Binaural Beats - Natural Height GrowthIsidro P. Buquiron100% (1)
- BAB I SomatoformDocument3 pagesBAB I SomatoformDewiRekmawatiPradaswariNo ratings yet
- HIV - AIDS PresentationDocument17 pagesHIV - AIDS PresentationphilNo ratings yet
- Health 8 Q3 Week 7-8 Module 1-6Document22 pagesHealth 8 Q3 Week 7-8 Module 1-6Richard CoderiasNo ratings yet
- CPC 0 Series QuestionsDocument6 pagesCPC 0 Series Questions19ucs175No ratings yet
- PROTOCOL of Management of Critical CasesDocument131 pagesPROTOCOL of Management of Critical Casesaziz.shokry.mosaNo ratings yet
- Necropsical DiagnosisDocument372 pagesNecropsical Diagnosistataru lauraNo ratings yet
- Heart Failure Infographic - Long Version - v1.0Document1 pageHeart Failure Infographic - Long Version - v1.0Oana-Adriana DutaNo ratings yet
- Clinical Teaching Plan SampleDocument9 pagesClinical Teaching Plan SampleElaine RetesNo ratings yet
- Retinal Hemorrhages Abusive Head Trauma or NotDocument6 pagesRetinal Hemorrhages Abusive Head Trauma or NotHercya IsabelNo ratings yet
- Lot 18 Cvab - Ce-.SemnatDocument24 pagesLot 18 Cvab - Ce-.SemnatEloy ColqueNo ratings yet
- Virtual Meeting House RulesDocument53 pagesVirtual Meeting House RulesJohana MedallaNo ratings yet