Professional Documents
Culture Documents
Alzheimer's Disease: Name: Pooja Adhikari Rollno: 27 SMTC
Uploaded by
sushma shrestha0 ratings0% found this document useful (0 votes)
139 views40 pageshj
Original Title
Alzheimer's disease
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documenthj
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
139 views40 pagesAlzheimer's Disease: Name: Pooja Adhikari Rollno: 27 SMTC
Uploaded by
sushma shresthahj
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 40
Alzheimer's disease
Name: pooja Adhikari
Rollno: 27
SMTC
Introduction
Alzheimer's disease is a progressive and irreversible
neurological brain disorder which is usually seen in
individuals older than 65 age. It affects the cells of
the brain and causes loss of memory, judgment and
changes in personality. It is also the most common
form of dementia, a group of disorders that impairs
mental functioning.
Cont..
• This disease was first described by Dr.Alois
Alzheimer, a German physician, in 1906.
• Memory loss is one of the earliest symptoms, along
with gradual decline of other intellectual and
thinking abilities, called cognitive functions and
changes in personality or behavior.
Epidemiology
Worldwide, nearly 50 million people have Alzheimer's or
related dementia. It is the 6th leading cause of death in the
united states(World Alzheimer's report, 2018).
Every year, around 4.6 million new dementia cases are
added in the existing pool of Alzheimer's disease with the
highest growth projections in china along with its south
Asian neighbors (World Health Organization [WHO],
2001).
About 3% of men and women ages 65 to 74 have
Alzheimer's disease, and nearly half of those ages 85
older may have this disease.
Stages of AD
Mild or Early Stage:
Friends, family and co workers begin to notice deficiencies.
Some common difficulties include:
Forgets names
Misplaces household items
Mild memory loss
Short attention span
Changes in the personality
Impaired judgment
Poor performance at work
Decline in ability to plan or organize
Cont..
Moderate or Middle Stage: Major gaps in
memory and deficits in cognitive function. Some
assistance with day to day activities becomes
essential. Some common difficulties include:
Disoriented to time, place and event
Agitated
Lose most awareness of recent experiences and
events as well as of their surroundings.
Tend to wander and become lost
Cont..
Unable to care for self
Irritable and anxious
Social isolation
Has difficulty in following simple instructions
Inability to recall important details such as their
current address, their telephone number etc.
Cont..
Severe or Late Stage:
This is the final stage of the disease when individuals
lose the ability to respond to their environment, the
ability to speak and the ability to control movement.
Unable to communicate
Does not recognize family
Incontinence of urine and feces
Loses the ability to stand and walk
Need full assistance with eating and toileting.
Causes
1.The exact cause of Alzheimer's disease is unknown.
2. However several factors are thought to be implicated
in this disease, Such as:
Age: Increasing age is the greatest known factor for
Alzheimer's disease. It is not a part of normal aging
but as we grow older the likelihood of developing AD
increases with the age.
Family history: People who have a parent or siblings
with Alzheimer's disease are more likely to get it
themselves.
Cont..
Environmental factors:
Cigarette smoking
Certain infections
Metals, industrials or other toxins
Use of cholesterol lowering drugs (statin).
Past head trauma: People who've had a severe head
trauma have a greater risk of Alzheimer's disease.
Poor sleep patterns: Research has shown that poor sleep
patterns such as difficulty falling asleep or staying asleep
increased the risk of Alzheimer's disease.
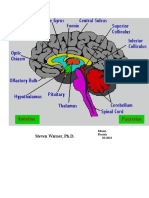
Pathophysiology
Alzheimer's disease attacks nerves and brain cells as
well as neurotransmitters. The destruction of these
parts causes clumps of protein to form around the
brain cells. These clumps are known as plaques and
bundles. The presence of these plaques and bundles
start to destroy more connections between the brain
cells, which makes the condition worse.
Cont…
Due to different etiological factors such as:
environmental factors, head trauma, certain
infections.
Changes occurs in the protein of the nerve cells of the
cerebral cortex.
Accumulation of the neuro fibrillary tangles and beta
amyloid plaques
Cont..
Neuro degeneration changes
Neuronal Function loss
Loss of memory function, cognitive and
intellectual impairment.
Ten Warning signs of AD
1. Memory loss
2. Difficulty in performing familiar tasks
3. Problems with language
4. Disorientation to time and place
5. Poor or decreased judgment
6. Misplacing things
7. Changes in mood or behavior
8. Changes in personality
9. Loss of initiative
10. Problems with abstract thinking
Symptoms
• Confusion
• Disturbances in short term memory
• Problems with attention
• Personality changes
• Language difficulties
• Unexplained mood swings.
Other Clinical features:
• Personality changes: lack of interest in day to day
activities, self centered, withdrawn, decreased self care.
• Memory impairment: Recent memory is prominently
affected.
• Cognitive impairment: Disorientation, poor judgment,
decreased attention span.
• Affective impairment: Irritableness, depression.
• Behavioral impairment: Stereotyped behavior,
alteration in sexual drives and activities, neurotic/
psychotic behavior.
Cont..
• Neurological impairment: Aphasia, agnosia,
seizures, headache.
• Sundowner syndrome: It is characterized by
drowsiness, confusion, ataxia; accidental falls may
occur at night when external stimuli such as light and
interpersonal orienting clues are diminished.
Diagnosis
1. History Taking
2. Physical Examination
3. Mini- Mental status Examination : shows cognitive
impairment.
4. CT- scan and MRI of the brain shows structural and
neurologic changes
5. gbCerebro gSpinal fluid Analysis : shows increased beta
amyloid deposits.
6. Electro encephalogram (EEG)
7. Electromyogram
8. Definitive diagnosis: Autopsy after death
Treatment
A. Pharmacological Treatment:
1. Acetyl cholinesterase inhibitors: Prevents the
breakdown of acetylcholine, a chemical messenger
important for learning and memory. Example:
Donepezil, Rivastigmine, Galantamine.
2. N- Methyl d- aspartate receptor antagonist
(NMDA): It is approved for moderate to severe
Alzheimer's disease treatment. Example: memantine.
Cont..
3. Anti Anxiety Drugs: It is used to treat agitation. It can
cause sleepiness, dizziness, falls so, they should be used for
short periods of time.
4. Antipsychotics Drugs : are sometimes used to treat
hallucinations, agitations and aggressions. Side effects of
these drugs can be serious including risk of death in some
older people with dementia. They should only be given to
people with Alzheimer's disease when the physician agrees
that the symptoms are severe.
5. Anticonvulsant Drugs: It is sometimes used to treat severe
aggression. Side effects may be sleepiness, dizziness, mood
swings etc.
Cont..
B. Nutrition:
People with Alzheimer's disease may forget to eat, lose
interest in preparing meals or does not eat a healthy
combination of foods. They may also forget to drink
enough, leading to dehydration and constipation. So,
they should be provided with high calorie, healthy
shakes of milk or other smoothies foods to prevent
difficulty in eating. Patients with AD should avoid
beverages with caffeine, which can increase with sleep
and trigger a frequent needs to urinate.
Cont..
C. Exercise
Regular exercise is an important part of a treatment plan.
Activities such as a daily walk can help to improve mood
and maintain the health of joints, muscles and the heart.
Exercise can also promote restful sleep and prevent
constipation.
D. Social engagement and activities: Social interactions
and activities can support the abilities and skills that are
preserved. Doing things that are meaningful and enjoyable
are important for the overall wellbeing of a person with
Alzheimer's disease.
Cont..
This may include:
- Listening to music or dancing
- Reading or listening to books
- Gardening or crafts
- Planned activities with children etc.
D. Coping and support: People with AD experience a
mixture of emotions like confusions, fear, anger, depression
etc. so, a calm and stable home environment can help to reduce
a behavior problems. The person should also be reassured that
life can be still enjoyed by providing support and doing the
best to help person too retain dignity and self respect.
Nursing Management
Assessment
1. Assess the health history and mental status
examination and physical examination, noting
symptoms indicating dementia.
2. Assess impaired memory or thinking( cognitive)
skills.
3. Assess the concentration and attention span with
awareness of time, place and person.
4. Assess the patients ability to cope with events,
interests in surroundings and activity motivation.
Cont..
5. Assess the effects of communication and deficits.
6. Assess patients for presence of wandering behavior
and specific reasons for wandering.
7. Assess the degree of impaired ability of competence,
emergence of impulsive behavior and decrease in
visual perception.
8. Assess patients surroundings for hazards and remove
them.
Nursing Diagnosis
1. Disturbed thought process related to chemical
imbalances in the brain as evidenced by
disorientation to time, place and circumstance.
2. Impaired verbal communication related to decreased
circulation to the brain as evidenced by confusion,
repetitive speech, stuttering or slurring speech.
3. Self care deficit related to cognitive and
neuromuscular impairment as evidenced by inability
to wash body parts and maintain appearance at
satisfactory levels.
Cont..
4. Impaired physical mobility related to dementia as
evidenced by decrease fine and gross motor
movement.
5. Disturbed sleep pattern related to Alzheimer's disease
progression as evidenced by sleeplessness and
fatigue.
6. Risk for injury related to decline in cognitive
function.
7. Anxiety related to confused thought process.
Nursing Intervention
A. Improving thought process:
1. Assess patient for depressive behaviors, causative
events and orient the patient to reality as warranted.
2. Establish a trusting relationship and permits the
patient to discuss topics that can help the patient to
deal with appropriate ways.
3. Use a non-judgmental attitude toward the patient and
actively listen to his feelings and concern.
4. Provide a calm, predictable environment to avoid
confusion and disorientation.
Cont..
B. Improving verbal communication:
1. Assess the patients ability to speak, language deficit,
cognitive or sensory impairment, presence of
aphasia, aphonia.
2. Instruct the patient to make a conscious effort to
speak slowly with deliberate attention to what the
listener are speaking.
3. Monitor the patient for non verbal communication
such as facial grimacing, smiling, crying, and
encourage the use of speech when possible.
Cont..
4. Remove competing stimuli and provide a clam,
unhurried atmosphere for communication.
5. Avoid rushing the patient when struggling to express
feelings and thoughts.
C. Promoting independence in self care
activities:
1. Determine the specific cause of each deficit such as
visual problems, weakness and cognitive impairment.
2. Provide positive reinforcement for all activities
attempted by the patients.
3. Render supervision for each activity until the patient
exhibits the skill effectively and is secured in
independent.
Cont..
4. Apply regular routines and allow adequate time for
the patient to complete task.
5. Guide the patient in accepting the needed amount of
dependence.
6. Maintain patients personal dignity and autonomy.
D. Promoting physical ability:
1. Teach the patient to concentrate on walking erectly.
2. Instruct the patient to perform a daily exercise that
will increase muscle strength.
3. Encourage the patient to raise the head of bed and
make position changes slowly.
4. Refer the patient to physical therapist.
5. Provide warm baths and massages.
E. Maintaining sleep pattern:
1.Assess patients sleep patterns and changes, naps,
frequency, amount of activity, number of time of
awakenings during night.
2. Ensure environment is calm, quiet, well ventilated and
absence of odor.
3. Monitor patients medications, use of alcohol and caffeine.
4. Provide backrubs, music and other relaxation techniques
before sleep.
5. Help patient to do exercises.
F. Promoting physical safety:
1. Provide a safe environment to allow the patient to
move freely as possible and relieves worry about
safety.
2. Prevent falls or other accidents by removing obvious
hazards and provide adequate lighting.
3. Prohibit driving.
4. Supervise all the activities outside the home to protect
the patient. As needed secure doors of the house.
5. Ensure that the patients wear an identification
bracelets or neck chain.
6. Avoid restraints because they may increase agitation.
7. Reduce the wandering behavior with gentle
persuasion and distraction.
G. Reducing anxiety and agitation:
1. Provide emotional support to reinforce a positive self
image.
2. Keep the environment simple, familiar and noise free,
limit changes.
3. Remain calm and unhurried while performing any
procedures or tasks to the patients.
4. Encourage patients to participate in simple activities or
hobbies.
5. Provide adequate rest and comfortable sleep.
Evaluation
• Maintained self care.
• Improved physical ability.
• Exhibits improved thought process.
• Improved sleep pattern.
• Improved verbal communication.
• Reduced anxiety levels.
Reference
1. Williams and wilkims, lippincott manual of nursing.
5th edition. Wolters kluwer(india)pvt.ltd. Newdelhi
page no: 175-177).
2. Brunner and siddharths, Textbook of Medical and
surgical nusring. 12th edition, 2013. walters
kluwer(india) pvt.ltd. Newdelhi.
3. Mandal, G.N(2019), Medical surgical nursing.
Crown point printing house pvt.ltd.
Thank you
You might also like
- Alzheimer S Disease and Related Dementias-2014Document34 pagesAlzheimer S Disease and Related Dementias-2014thuhvoNo ratings yet
- Alzheimer's Disease Nursing Care Plan & ManagementDocument6 pagesAlzheimer's Disease Nursing Care Plan & ManagementBryan NguyenNo ratings yet
- Alzheimer's DiseaseDocument6 pagesAlzheimer's DiseaseDelia Lingcong100% (1)
- ALZHEIMERDocument9 pagesALZHEIMERKhem Limoso100% (2)
- Neurological AssessmentDocument61 pagesNeurological AssessmentSamantha SunglaoNo ratings yet
- Alzheimer's DiseaseDocument18 pagesAlzheimer's DiseaseakshayNo ratings yet
- CVADocument13 pagesCVAAmlan jyoti thanapatiNo ratings yet
- Brain AbscessDocument27 pagesBrain AbscessFitrie Desbassarie100% (1)
- Stress Management: Rajesh Kumar Sharma Asso Professor HCN, SrhuDocument73 pagesStress Management: Rajesh Kumar Sharma Asso Professor HCN, SrhuRajesh SharmaNo ratings yet
- Neurologicdisorders 100816033614 Phpapp01 PDFDocument96 pagesNeurologicdisorders 100816033614 Phpapp01 PDFenam professorNo ratings yet
- Geriatric SyndromsDocument26 pagesGeriatric SyndromsMOC NAJRAN100% (1)
- Acute Myocardial InfarctionDocument22 pagesAcute Myocardial InfarctionkpsuanNo ratings yet
- DeliriumDocument2 pagesDeliriumAngelique van Tonder100% (2)
- Presented By: VIVEK DEVDocument38 pagesPresented By: VIVEK DEVFranchesca LugoNo ratings yet
- Approach To Unconsious PTDocument62 pagesApproach To Unconsious PTHussain AzharNo ratings yet
- AlzheimerDocument7 pagesAlzheimerInas100% (1)
- Dementia Power PointDocument23 pagesDementia Power Pointapi-253856690No ratings yet
- Promoting Personal Hygiene & Promoting Rest & SleepDocument26 pagesPromoting Personal Hygiene & Promoting Rest & SleepYousef JafarNo ratings yet
- UnconsciousnessDocument15 pagesUnconsciousnesssippuNo ratings yet
- Geriatric NursingDocument46 pagesGeriatric NursingQuolette Constante100% (2)
- Organic Brain DisorderDocument69 pagesOrganic Brain DisorderHowell Mathew100% (1)
- Geria (Midterms)Document42 pagesGeria (Midterms)ANGELA GLORIA LAPUZNo ratings yet
- Understanding Alzheimer's DiseaseDocument10 pagesUnderstanding Alzheimer's DiseaseRiaNo ratings yet
- Glasgow Coma Scale classifications and limitationsDocument3 pagesGlasgow Coma Scale classifications and limitationsEleanorNo ratings yet
- Assessment of The IntegumentaryDocument3 pagesAssessment of The IntegumentaryMona ArabiaNo ratings yet
- Head Trauma & Management: Dr. Utham Murali. M.S M.B.A. Asso - Prof of Surgery IMS / MSU / MalaysiaDocument48 pagesHead Trauma & Management: Dr. Utham Murali. M.S M.B.A. Asso - Prof of Surgery IMS / MSU / MalaysiaNinaNo ratings yet
- Promoting Safety in Healthcare EnvDocument13 pagesPromoting Safety in Healthcare EnvnamNo ratings yet
- AlzheimersDocument9 pagesAlzheimersNader Smadi100% (1)
- By Pajanustan, Ben David B.Document27 pagesBy Pajanustan, Ben David B.Ben DavidNo ratings yet
- Degenerative Neurologic DisordersDocument29 pagesDegenerative Neurologic DisordersVIDYANo ratings yet
- Approach To An Unconscious Patient-OyeyemiDocument41 pagesApproach To An Unconscious Patient-OyeyemiOyeyemi AdeyanjuNo ratings yet
- Enema AdministrationDocument16 pagesEnema AdministrationEmerald IsleNo ratings yet
- Infection Control ModuleDocument12 pagesInfection Control ModuleFreida Michelle BonnitNo ratings yet
- Therapeutic Nurse RelationshipsDocument20 pagesTherapeutic Nurse RelationshipsKatie McFarlandNo ratings yet
- Foreigh Body Airway Obstruction Management July 2019Document1 pageForeigh Body Airway Obstruction Management July 2019Feliros S. SanciangcoNo ratings yet
- NCM 116 Module 3 and 4 PDFDocument183 pagesNCM 116 Module 3 and 4 PDF7rvcnnxk88No ratings yet
- Neurology - : Approach To Headache DisordersDocument8 pagesNeurology - : Approach To Headache DisordersKarenNo ratings yet
- Top Comfort and Safety Devices Used in HospitalsDocument9 pagesTop Comfort and Safety Devices Used in HospitalsaibutyNo ratings yet
- Bedbath & Perineal CareDocument22 pagesBedbath & Perineal CarealelichengNo ratings yet
- Urinary CatheterizationDocument2 pagesUrinary CatheterizationFains YdbwidNo ratings yet
- Cerebrovascular DiseaseDocument29 pagesCerebrovascular DiseaseKamsha UyNo ratings yet
- Chapter 12 Palliative CareDocument49 pagesChapter 12 Palliative Careapi-545172676No ratings yet
- Gastrointestinal DrugsDocument2 pagesGastrointestinal DrugsJannah Mikhaela Alibay VillarinNo ratings yet
- Assessing The Ear and HearingDocument32 pagesAssessing The Ear and HearingArlyn Mendenilla0% (1)
- Bone Marrow and Stem Cell TranspplantDocument28 pagesBone Marrow and Stem Cell TranspplantVILLEJO JHOVIALENNo ratings yet
- Alzheimeru2019s DiseaseDocument17 pagesAlzheimeru2019s Diseaseapi-262538456100% (1)
- Colostomy CareDocument4 pagesColostomy CareRhenzes HaraNo ratings yet
- Care of Older Adult Full Notes For Next Weeks QuizDocument14 pagesCare of Older Adult Full Notes For Next Weeks QuizMercy Anne EcatNo ratings yet
- CHF Drugs Guide: Key Medications for Treating Congestive Heart FailureDocument21 pagesCHF Drugs Guide: Key Medications for Treating Congestive Heart Failuremohsen mirdamadiNo ratings yet
- NCM103 (FUNDA) Module 1 Concept of NursingDocument4 pagesNCM103 (FUNDA) Module 1 Concept of NursingJohn Joseph CruzNo ratings yet
- OT6 - Amyotrophic Lateral SclerosisDocument19 pagesOT6 - Amyotrophic Lateral SclerosisAnnbe BarteNo ratings yet
- Dementia & DeliriumDocument170 pagesDementia & Deliriummengaku0% (1)
- DEMENTIADocument42 pagesDEMENTIAputri maharaniNo ratings yet
- GB SyndromeDocument17 pagesGB Syndromehajra StudentNo ratings yet
- Geria UNIT 3Document5 pagesGeria UNIT 3Raiden VizcondeNo ratings yet
- Procedure Manual Med SurgDocument15 pagesProcedure Manual Med SurgTina AlteranNo ratings yet
- Nursing Care of The Older Patient in Chronic IllnessDocument40 pagesNursing Care of The Older Patient in Chronic IllnessMaggay LarsNo ratings yet
- What Is A Psychological DisorderDocument28 pagesWhat Is A Psychological DisorderJoey VigonteNo ratings yet
- Alzheimer's Disease Diagnosis and StagesDocument32 pagesAlzheimer's Disease Diagnosis and StagesPC LaptopNo ratings yet
- Alzheimer's Dis-WPS OfficeDocument12 pagesAlzheimer's Dis-WPS OfficeDavid MharkNo ratings yet
- Z-Test For Single MeanDocument32 pagesZ-Test For Single Meansushma shresthaNo ratings yet
- Purbanchal University Shree Medical and Technical College Bharatpur 10, ChitwanDocument10 pagesPurbanchal University Shree Medical and Technical College Bharatpur 10, Chitwansushma shresthaNo ratings yet
- Palliative Care in Non Cancer Patients NotesDocument19 pagesPalliative Care in Non Cancer Patients Notessushma shresthaNo ratings yet
- Presentation 1Document2 pagesPresentation 1sushma shresthaNo ratings yet
- Bharatpur Hospital Nursing College Bharatpur-10, Chitwan Subject: Fundamental of Nursing Unit TestDocument3 pagesBharatpur Hospital Nursing College Bharatpur-10, Chitwan Subject: Fundamental of Nursing Unit Testsushma shresthaNo ratings yet
- News Orint NoteDocument2 pagesNews Orint Notesushma shresthaNo ratings yet
- Nursing Process: A Critical Thinking ToolDocument15 pagesNursing Process: A Critical Thinking Toolsushma shresthaNo ratings yet
- 18.2 Pain Management - PBNDocument21 pages18.2 Pain Management - PBNsushma shresthaNo ratings yet
- Sigmoidoscopy: Presented by Kriti Adhikari Roll No: 17Document38 pagesSigmoidoscopy: Presented by Kriti Adhikari Roll No: 17sushma shresthaNo ratings yet
- Chest Xray 2Document39 pagesChest Xray 2sushma shresthaNo ratings yet
- Retinal Vascular DisordersDocument52 pagesRetinal Vascular Disorderssushma shresthaNo ratings yet
- Anatomy and PhysiologyDocument42 pagesAnatomy and Physiologysushma shresthaNo ratings yet
- Drugs For Cancer Patients: Mona Shrestha MN (Adult Nursing)Document77 pagesDrugs For Cancer Patients: Mona Shrestha MN (Adult Nursing)sushma shresthaNo ratings yet
- Psychosocial Communication Palliative CareDocument49 pagesPsychosocial Communication Palliative Caresushma shresthaNo ratings yet
- Welcome To Presentation: Presented by Karishma Mahato Roll No. 15Document18 pagesWelcome To Presentation: Presented by Karishma Mahato Roll No. 15sushma shresthaNo ratings yet
- Chest Xray 2Document39 pagesChest Xray 2sushma shresthaNo ratings yet
- Intravenous Urography (IVU)Document35 pagesIntravenous Urography (IVU)sushma shresthaNo ratings yet
- Presentation on Cerebral Angiography and EEG ProceduresDocument25 pagesPresentation on Cerebral Angiography and EEG Proceduressushma shresthaNo ratings yet
- EsophagusDocument72 pagesEsophagussushma shresthaNo ratings yet
- Anatomy and Treatment of EntropionDocument34 pagesAnatomy and Treatment of Entropionsushma shrestha100% (1)
- Corneal Ulcer: Prepared By: Renuka Shrestha Roll No: 29 PBBN 3rd Year SMTCDocument41 pagesCorneal Ulcer: Prepared By: Renuka Shrestha Roll No: 29 PBBN 3rd Year SMTCsushma shresthaNo ratings yet
- Retinal Vascular DisordersDocument52 pagesRetinal Vascular Disorderssushma shresthaNo ratings yet
- Catheterization GuideDocument28 pagesCatheterization Guidesushma shresthaNo ratings yet
- Alzheimer's Disease: Name: Pooja Adhikari Rollno: 27 SMTCDocument40 pagesAlzheimer's Disease: Name: Pooja Adhikari Rollno: 27 SMTCsushma shresthaNo ratings yet
- Presentation On MeningitisDocument51 pagesPresentation On Meningitissushma shresthaNo ratings yet
- Chest Tube Insertion GuideDocument39 pagesChest Tube Insertion Guidesushma shresthaNo ratings yet
- Trichiasis: Prepared By:pooja Adhikari Roll No.: 27 SMTCDocument27 pagesTrichiasis: Prepared By:pooja Adhikari Roll No.: 27 SMTCsushma shresthaNo ratings yet
- Corneal Ulcer: Prepared By: Renuka Shrestha Roll No: 29 PBBN 3rd Year SMTCDocument41 pagesCorneal Ulcer: Prepared By: Renuka Shrestha Roll No: 29 PBBN 3rd Year SMTCsushma shresthaNo ratings yet
- Modified Curriculum: Use of Restraints Precautions Danger Associated With RestraintsDocument3 pagesModified Curriculum: Use of Restraints Precautions Danger Associated With Restraintssushma shresthaNo ratings yet
- LA Prediction Dec 10th To Dec 16th 2022 PDFDocument375 pagesLA Prediction Dec 10th To Dec 16th 2022 PDFSahil MishraNo ratings yet
- How Music Boosts Brain Health in Many WaysDocument4 pagesHow Music Boosts Brain Health in Many WaysDani Ursaiche100% (1)
- Language and The Human BrainDocument2 pagesLanguage and The Human BrainDharshan GunaNo ratings yet
- Mesolimbic Vs NigrostriatalDocument7 pagesMesolimbic Vs NigrostriatalAmrit SoniaNo ratings yet
- Estudios de Psicología: Studies in PsychologyDocument18 pagesEstudios de Psicología: Studies in PsychologySebastian Gonzalez MazoNo ratings yet
- Biology of The MindDocument3 pagesBiology of The MindrinieroxNo ratings yet
- Building Self-Compassion - 03 - Preparing For Self-CompassionDocument9 pagesBuilding Self-Compassion - 03 - Preparing For Self-CompassionThe Happy Mind HouseNo ratings yet
- Ond Vidyalaya ke Pradhan ka PustakDocument33 pagesOnd Vidyalaya ke Pradhan ka PustakSanjiv GautamNo ratings yet
- Sts Cheat Sheet of The BrainDocument30 pagesSts Cheat Sheet of The BrainRahula RakeshNo ratings yet
- Psychology 4th Edition Schacter Test BankDocument86 pagesPsychology 4th Edition Schacter Test BankdawnholmesrtcongdbszNo ratings yet
- Neuroscience and The SoulDocument5 pagesNeuroscience and The SoulMatija GubecNo ratings yet
- Are Sex-Related Category-Specific Differences in Semantic Tasks Innate or Influenced by Social Roles?Document9 pagesAre Sex-Related Category-Specific Differences in Semantic Tasks Innate or Influenced by Social Roles?argiaescuNo ratings yet
- Cognition Matlin 7th TBDocument22 pagesCognition Matlin 7th TBDevin MckayNo ratings yet
- Kalinowski 2003Document9 pagesKalinowski 2003GabyMillahuequeQuijadaNo ratings yet
- The Neural Basis of ReadingDocument362 pagesThe Neural Basis of ReadingomegarmxNo ratings yet
- Imagery and Training The Minds Eye - Lee PulosDocument12 pagesImagery and Training The Minds Eye - Lee Pulosmugume ignatius100% (2)
- Brain Cases that Shaped NeuroscienceDocument12 pagesBrain Cases that Shaped NeuroscienceShania Christie TumilaarNo ratings yet
- EEG PresentationDocument39 pagesEEG PresentationAlfred Fredrick100% (1)
- Human: CommunicationDocument27 pagesHuman: CommunicationazharaallanNo ratings yet
- PSY396S Neurochemical Basis of BehaviourDocument5 pagesPSY396S Neurochemical Basis of BehaviourCaio OliveiraNo ratings yet
- Brain Herniation SyndromeDocument28 pagesBrain Herniation SyndromeSarahScandy100% (4)
- 7 Communication Do's and Don'ts For Leaders Facing Rapid Organizational ChangeDocument10 pages7 Communication Do's and Don'ts For Leaders Facing Rapid Organizational ChangeAnshumali Saxena100% (1)
- Attachment Style QuestionnaireDocument5 pagesAttachment Style QuestionnaireCristina GhenofNo ratings yet
- Neural Networks: A New Technique For Development of Decision Support Systems in DentistryDocument5 pagesNeural Networks: A New Technique For Development of Decision Support Systems in DentistryOussema GazzehNo ratings yet
- Teens Brain Under ConstructionDocument12 pagesTeens Brain Under ConstructionDoru-Mihai Barna100% (2)
- LC #6Document33 pagesLC #6Vannie CalugayNo ratings yet
- Bibliografie UBB PsihologieDocument2 pagesBibliografie UBB PsihologieAdina CarterNo ratings yet
- The Student S Guide of Social NeuroscienciaDocument433 pagesThe Student S Guide of Social NeuroscienciasilviagarciatoledoNo ratings yet
- Research PaperDocument11 pagesResearch PaperEllaina SwallowsNo ratings yet
- Sex Differences in Brain Anatomy - National Institutes of Health (NIH)Document4 pagesSex Differences in Brain Anatomy - National Institutes of Health (NIH)Ryan BurtonNo ratings yet