Professional Documents
Culture Documents
Emphysema
Emphysema
Uploaded by
Daphnie EstacioOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Emphysema
Emphysema
Uploaded by
Daphnie EstacioCopyright:
Available Formats
DAPHNIE MAE ESTACIO
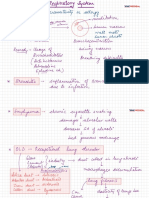
COPD: EMPHYSEMA
Environmental: Long Term
Genetic Predesposition: A-1
exposure to cigarette smoke or
Antitrypsin deficiency
pollution
Increased
inactivation of lung
neutrophils elastase an Free Radicals
proteases
matrix proteases
Degrades Elastin by
Lung Inflammation:
Proteolysis
Incresed oxidative stress,
inflammatoruy cytokines
an protease function
Destruction od
alevolar walls and
capillaries Proteolytic destruction
of Lung parenchyma
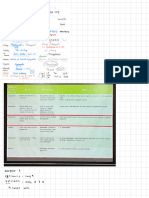
ABG: pH 7.34 Risk for Activity Intolerance r/t
PaCO2: 47.92 imbalance between oxygen supply and
HCO3: 27.19 meq demand
Decreased Lung Respiratory
ability to prevent damage Acidocis
to lung tissue Diagnostic:
Monitor and record clients ability to tolerate activity, note
changes in the Vital Signs
Assess the client daily for appropriateness of activity
and bed orders.
Therapeutic:
Total Expiration Lungs don't fully More CO2 remains Provide emotional support and encouragement to the
Decreased Elastic client
takes longer time than emply and air is trapped and diffuses into the Hypoxemia
recoil to push air Refer the client to physical therapy to help increase
normal in the alveoli blood
ABG: pH 7.34 activity levels.
PaCO2: 47.92
HCO3: 27.19 meq Educative:
Teach the patient to avoid activities that causes fatigue
Prolonged
Expiration Enlarged air spaces Lung hyperinflation
impaired gas exchange related to
Ventilation-perfusion imbalance
Increased lung
Decreased Lung volume means
Diagnostics:
Compliance diaphragm is tonically Monitor Respiratory rate. depyth, eases of respiration,
contracted
watch out for use of accessory muscles
Note Pattern of respiration
Assess Breath sound, noting adventitious breath sounds.
Diaphragm can't
Risk for Activity Intolerance r/t Monitor oxygen saturation frequently.
Low Ventilation and flatten much further to
fatigue or weakness Oserve for cyanosis
Low perfusion generate deep breaths
Therapeutic:
Administer Oxygen therapy as odered
Diagnostic: Fatigue Position the patient in an upright or semi fowlers position
Determince ability of the client to perform ADL Increased Work of Help patient to take deep breathing .
or generalized
Monitor oxygen saturation, respiratory rate, pulse rate. Breathing to ventilate
weakness Rapid and Shallow
larger lung Eductive:
Breathing
Therapeutic: Teach the patient pursed lip breathing
Yes
Ensure that the client will perform activities that will not
compromise their condition. Collaborative:
RR: 30 CPM
Promote adequate rest . DYSPNEA Refer COPD client to a pulmonary rehabilitation program
Decreased Fluid Intake
Educative:
Shortness of Breath
Teach the client techniques such as controlled
on exertion , O2 Sat:
breathing techniques Ineffective Breathing
87%
Patten realated to
respiratory muscle fatigue
Dehydration
Diagnostics:
HCT: 70% Monitor Respiratory rate. depyth, eases of respiration
Note Pattern of respiration
Assess Breath sound, noting adventitious breath
sounds.
Monitor oxygen saturation frequently.
Deficient Fluid Volume r/t
inadequate fluid intake Therapeutic:
Administer Oxygen therapy as odered
Position the patient in an upright or semi fowlers position
Encourage patient to take deep breaths as prescribed
Diagnostic:
intervals.
Monitor total fluid intake and output every 4 hours
Observe fot dry tongue and mucous membranes
Eductive:
Monitor pulse, respiratory, and blood pressure.
Teach the patient pursed lip breathinh
Check skin turgor of the client
Help client identify an emergency plan .
Therapeutic:
Provide fluid replacement as per doctors order
Encourage patient to take sips of water frequently
Offer foods that
taht contains high amount of fluid in them.
Educative:
Teach the patient the importance of hydration.
You might also like
- Modified 9 BreathsDocument24 pagesModified 9 BreathsRyan Burton100% (1)
- Types of PneumothoraxDocument13 pagesTypes of PneumothoraxumarNo ratings yet
- Hormones: College of Arts and Sciences Norzagaray CollegeDocument48 pagesHormones: College of Arts and Sciences Norzagaray CollegeKristopher OngNo ratings yet
- ARDS Concept Map - BunayogDocument2 pagesARDS Concept Map - BunayogJacela Annsyle BunayogNo ratings yet
- Pcap PathophysiologyDocument3 pagesPcap PathophysiologyZandra Lyn AlundayNo ratings yet
- 13 BDocument38 pages13 BBruno100% (4)
- NCM 112 - Practice TestDocument6 pagesNCM 112 - Practice TestUzumaki K100% (1)
- PiperacillinDocument3 pagesPiperacillinMario Magtaka0% (1)
- NCP PcapDocument2 pagesNCP PcapKenj Pereña100% (1)
- Biology For You Intro and Answers To Further QuestionsDocument49 pagesBiology For You Intro and Answers To Further QuestionsSweetygirl_1646% (13)
- NCP Ineffective Tissue Perfusion and Self Care DeficitDocument5 pagesNCP Ineffective Tissue Perfusion and Self Care DeficitFrances Anne Pasiliao100% (3)
- Chi Nei Tsang IDocument9 pagesChi Nei Tsang Ijuanitos111No ratings yet
- Cell CycleDocument1 pageCell CycleAvinashNo ratings yet
- MK: Ketidakefektifan Bersihanjalanna Pas: - EKG: Sinus Takikardi - X-Ray:pemebesaranparu, DiafragmamendatarDocument2 pagesMK: Ketidakefektifan Bersihanjalanna Pas: - EKG: Sinus Takikardi - X-Ray:pemebesaranparu, DiafragmamendatarpetriNo ratings yet
- Pathophysiology of PUDDocument2 pagesPathophysiology of PUDdeoxis1933% (3)
- Pathophysiology of PUDDocument2 pagesPathophysiology of PUDLEAH LUZADANo ratings yet
- ANSpharmacologyDocument1 pageANSpharmacologyUsmleNo ratings yet
- Summary of Pharmacology1 by 3alam El Teb DR - MahmoudDocument41 pagesSummary of Pharmacology1 by 3alam El Teb DR - MahmoudaamirNo ratings yet
- Summary Pharmaco - Pathology MSKDocument6 pagesSummary Pharmaco - Pathology MSKminkcd51No ratings yet
- Trizol InfographicsDocument1 pageTrizol InfographicsmuhammadhanifmohdfahmiNo ratings yet
- WS1979 FactorsDocument18 pagesWS1979 FactorssheraNo ratings yet
- Adrenal Gland Cortisol Illustration AtfDocument1 pageAdrenal Gland Cortisol Illustration Atf2ymyccmvfcNo ratings yet
- DrugsDocument1 pageDrugsrkh647m7szNo ratings yet
- Mind MapDocument1 pageMind MapPatiphan PeeyuhaNo ratings yet
- Drugs Inhibiting Cell Wall Synthesis - 2Document6 pagesDrugs Inhibiting Cell Wall Synthesis - 2NeelabhNo ratings yet
- Pharma Complete PPDocument103 pagesPharma Complete PPHamza KhanNo ratings yet
- Almanda Gitta PuspaDocument1 pageAlmanda Gitta PuspaAlmanda Gitta PuspaNo ratings yet
- SF2 - Lecture-03 - Cell The Unit of Life - NotesDocument11 pagesSF2 - Lecture-03 - Cell The Unit of Life - Notesdisha shuklaNo ratings yet
- Thrombolytics-1Document3 pagesThrombolytics-1Shayan ShayanNo ratings yet
- 3rd Year Drugs ShizzaeDocument3 pages3rd Year Drugs ShizzaeMatheesha HerathNo ratings yet
- All BacteriaDocument14 pagesAll Bacteriamorale28100% (2)
- Ehambutol Inhibits Mycobacterial Arabinosyltransferase Streptomcin Binds To 16s rRNA of BacteriaDocument1 pageEhambutol Inhibits Mycobacterial Arabinosyltransferase Streptomcin Binds To 16s rRNA of Bacteriakamil malikNo ratings yet
- Patho 1aDocument3 pagesPatho 1aaaaalliah2No ratings yet
- Learning TaskDocument4 pagesLearning TaskROSEMARIE ONGNo ratings yet
- Acetyl Cyst EineDocument3 pagesAcetyl Cyst EineCen Janber CabrillosNo ratings yet
- Mitochondria: All Respiration Processes Occur Here, Except Glycolysis Outer Mitochondrial MembraneDocument1 pageMitochondria: All Respiration Processes Occur Here, Except Glycolysis Outer Mitochondrial MembraneAuriceliaOliveiraNo ratings yet
- OncogenesDocument1 pageOncogenesAqiena BalqisNo ratings yet
- FiguresDocument2 pagesFiguresRhythm MilanNo ratings yet
- Chemistry A Level - Nitrogen - SulfurDocument2 pagesChemistry A Level - Nitrogen - SulfurKeanan WongsoNo ratings yet
- هاشمDocument2 pagesهاشمHashim OmarNo ratings yet
- Pictorial Essay: Postpneumonectomy ComplicationsDocument9 pagesPictorial Essay: Postpneumonectomy ComplicationsMurali BalaNo ratings yet
- CNS: Headach E, Dizzines S, Vertigo, Nerve Root Lesion, Asthenia, InsomniDocument8 pagesCNS: Headach E, Dizzines S, Vertigo, Nerve Root Lesion, Asthenia, InsomniHsintan HsuNo ratings yet
- Condensed Note - HematoDocument4 pagesCondensed Note - HematoTanawit SaisriNo ratings yet
- Expression Vector, Baculovirus Expression Vector: Promila Sheoran Ph.D. Biotechnology GJU S&T HisarDocument18 pagesExpression Vector, Baculovirus Expression Vector: Promila Sheoran Ph.D. Biotechnology GJU S&T HisarYooobsan Nii barriitiNo ratings yet
- Safari - Jun 23, 2023 at 10:35 AMDocument1 pageSafari - Jun 23, 2023 at 10:35 AMBianca LozanoNo ratings yet
- Molecular Basis of Inheritance MindDocument1 pageMolecular Basis of Inheritance MindNetflix BabaNo ratings yet
- Disseminated Intravascular CoagulationDocument1 pageDisseminated Intravascular CoagulationAnn Justine OrbetaNo ratings yet
- Hepatitis BDocument6 pagesHepatitis BCarmen MargoNo ratings yet
- B6 Molecular Basis of InheritanceDocument1 pageB6 Molecular Basis of InheritancefunbytesytNo ratings yet
- Endocrine Physiology - 24. Male Reproductive System - Spermatogenesis - KeyDocument1 pageEndocrine Physiology - 24. Male Reproductive System - Spermatogenesis - Keyranag59100No ratings yet
- Cell Biology) 7. DNA Structure - Organization - KeyDocument1 pageCell Biology) 7. DNA Structure - Organization - KeyLeen AlhussainNo ratings yet
- Cell FunctionsDocument1 pageCell Functionsapi-287186989No ratings yet
- DiareDocument1 pageDiarejumraaqabah382No ratings yet
- Drug StudyDocument4 pagesDrug StudyMc Cobert AlipioNo ratings yet
- Components of BloodDocument1 pageComponents of BloodnaduniNo ratings yet
- Modern Treatment Star Comprehensive Insurance PolicyDocument1 pageModern Treatment Star Comprehensive Insurance PolicyYashwanth KrishnanNo ratings yet
- GastroDocument9 pagesGastroJoshua AtienzaNo ratings yet
- Pulmonary Tuberculosis PathophysiologyDocument1 pagePulmonary Tuberculosis PathophysiologyMIR SARTAJNo ratings yet
- Notes 3Document2 pagesNotes 3kiarabravo1226No ratings yet
- SF1-Lecture-03 - Breathing and Exchange of Gases NotesDocument7 pagesSF1-Lecture-03 - Breathing and Exchange of Gases Notesdisha shuklaNo ratings yet
- InflammationDocument1 pageInflammationmp658t952dNo ratings yet
- Exocytosis and Endocytosis: How Are Vesicles Formed? Vesicles Look Similar by Electron MicrosDocument4 pagesExocytosis and Endocytosis: How Are Vesicles Formed? Vesicles Look Similar by Electron MicrosRicky ShahNo ratings yet
- Proteine - FiziopDocument4 pagesProteine - FiziopAndreea IlincaNo ratings yet
- Components of Cell-Matrix Adhesions: Cell Science at A Glance 3577Document3 pagesComponents of Cell-Matrix Adhesions: Cell Science at A Glance 3577Andres F. TorresNo ratings yet
- Carbapenems Monobactam Glycopeptide Lipopeptide Tetracycline Penicillins CephalosporinsDocument8 pagesCarbapenems Monobactam Glycopeptide Lipopeptide Tetracycline Penicillins CephalosporinsBrandon Georges (Scribblemeascript)No ratings yet
- Build A Cell Card Game WorksheetDocument2 pagesBuild A Cell Card Game WorksheetlibrahimliNo ratings yet
- Build A Cell Card Game WorksheetDocument2 pagesBuild A Cell Card Game WorksheetSu AlghNo ratings yet
- Sickle Cell Anaemia by SALDocument4 pagesSickle Cell Anaemia by SALSahar Ahmed LaskarNo ratings yet
- PulmonologyDocument175 pagesPulmonologyJohanna GarciaNo ratings yet
- Take A Deep BreathDocument5 pagesTake A Deep BreathMelanie DeivenNo ratings yet
- COPD Spirometry ModuleDocument50 pagesCOPD Spirometry ModuleMeydita MahardiNo ratings yet
- Quarter 2, Week 3 - NOVEMBER 21-25, 2022Document28 pagesQuarter 2, Week 3 - NOVEMBER 21-25, 2022MARK GIL SALVINONo ratings yet
- Jurnal Tension Pneumotoraks PDFDocument6 pagesJurnal Tension Pneumotoraks PDFNaNa HunNo ratings yet
- 4 Pulmonary Rehab ContentDocument24 pages4 Pulmonary Rehab ContentRamiro Avendaño RebolledoNo ratings yet
- CPL Human Performance and Limitations ManualDocument150 pagesCPL Human Performance and Limitations ManualChina LalaukhadkaNo ratings yet
- Unacadmey Basic Organic Chemistry PDFDocument92 pagesUnacadmey Basic Organic Chemistry PDFAbhishek VermaNo ratings yet
- Nursing Case CadDocument26 pagesNursing Case CadShield DalenaNo ratings yet
- Respiratory SystemDocument9 pagesRespiratory SystemAtif JavaidNo ratings yet
- Integrated Science Year 1Document45 pagesIntegrated Science Year 1Andre Swaggerific PickettNo ratings yet
- JBLNPairwayDocument39 pagesJBLNPairwayjmscribblerNo ratings yet
- ParagraphDocument2 pagesParagraphAninditaElfaNo ratings yet
- Meditating With Yantras Breathing ExercisesDocument6 pagesMeditating With Yantras Breathing ExercisesrocknandNo ratings yet
- Nursing Care of Patients With Pneumothorax: Prepared By: N. WadeDocument33 pagesNursing Care of Patients With Pneumothorax: Prepared By: N. WadeokaciaNo ratings yet
- Difference Between Smokers and Non SmokersDocument9 pagesDifference Between Smokers and Non SmokersMohammad MashhoodNo ratings yet
- UNIT 1 Biomedical EngineeringDocument128 pagesUNIT 1 Biomedical EngineeringgajulasureshNo ratings yet
- M.Sc. II Sem. (Zoology) : Primitive Characters of DipnoiDocument11 pagesM.Sc. II Sem. (Zoology) : Primitive Characters of DipnoirajuNo ratings yet
- Leader Live Minor-01 14 May QPDocument23 pagesLeader Live Minor-01 14 May QPkavyasaxena107No ratings yet
- English TB Paru SGD 9 Malika Sayyidina Azizah HakimDocument8 pagesEnglish TB Paru SGD 9 Malika Sayyidina Azizah HakimbruhwahatNo ratings yet
- Geriatric Considerations in Nursing: Priyanka. T M SC Nursing 1 YearDocument70 pagesGeriatric Considerations in Nursing: Priyanka. T M SC Nursing 1 Yearsanthiyasandy100% (1)