Professional Documents
Culture Documents
Epidermis: - Five Sub-Layers of The Epidermis
Uploaded by
Pau De GuzmanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Epidermis: - Five Sub-Layers of The Epidermis
Uploaded by
Pau De GuzmanCopyright:
Available Formats
Dermatology • Epidermis
The Skin – The outermost layer of skin made up of
stratified, or layered, tissue
• Largest organ in the body
– The thinnest layer of skin and the first
• Performs many functions to protect the body barrier of protection against foreign
– Regulates body temperature substances entering the body
– Maintains water and electrolyte – Keratinocytes – the principal cells of
balance the epidermis
– Focal point of the body’s sense of – Skin cells are produced by mitosis, the
touch, temperature, and pain basic process of cell division and
producing new cells
– Defends the body against infection
– Desquamation is the process of
– Shields the body from the sun’s harmful replacing dead skin cells with new cells
effects from deeper layers below
– Protects the body’s deeper tissues from
injury
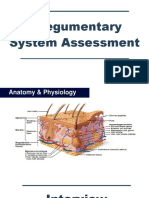
Anatomy of the Skin
• Skin collectively is referred to as integument
• Integumentary system consists of:
– Skin
– Its accessory structures (hair, sweat
glands)
• Five sub-layers of the epidermis:
– Underlying tissue
– Bottom layer—stratum germinativum
• Cutaneous describes something relating to the (basal layer)
skin
• Made up of basal cells and
Three layers: Epidermis, dermis, and subcutaneous melanocytes that produce
melanin, the pigment that
makes up skin color
– Stratum spinosum (spiny layer)
– Stratum granulosum (grainy layer)
– Stratum lucidum (clear layer)
– Stratum corneum (uppermost, horny
layer)
• Contains mostly dead skin cells
• Dermis HAIR
—Second Layer, often called “true skin” – Composed of dead epithelial cells
Contains: – Contains varying amounts of melanin
for color
- Collagen and fibrillin that gives elasticity,
tone, and strength to skin – The root ends in a bulb, which is lodged
- Nerve endings, hair follicles, and blood in a pit in the skin called a follicle
vessels
– Each follicle gives rise to a single hair –
- Immune cells that defend the body against
foreign invaders the skin of the average adult contains about
5 million hairs
- Papillary layer, where epidermis and dermis
meet
• Subcutaneous Layer NAILS
—Third Layer – Develop from the epidermis and
protect the tips of the fingers and toes
– Subcutaneous means “beneath the
skin” – Lunula: the white half-moon shape
located on top of the nail at the proximal
– Also called the “fat layer”
end of the nail bed
– Fastens the skin to the underlying body
surface
– Stores most body fat
– Paronychia: a bacterial infection caused
by biting or tearing the skin at the side or
base of a fingernail
– Onychomycosis: a fungal infection of
the nail
GLANDS: 2 Types
• Exocrine glands, which drain
secretions through ducts, or tubes
• Two types of exocrine glands: Common Dermatologic Disorders and Treatments
• Rash: Also called rubor, is an inflammation in
• Sebaceous glands open into hair the skin that affects its appearance or texture
follicles and secrete sebum, which – Symptoms of rash:
softens and lubricates the skin • Erythema (redness)
• Pruritus (itching)
• Sebaceous cyst: a sebaceous
• Edema (swelling)
gland that becomes blocked
• Hives (urticaria)
with sebum
• Dermatitis: an inflammation of the upper layers
• Sweat glands secrete a watery fluid of the skin that results in a rash
(sweat) in response to heat or – Types of dermatitis:
sometimes to emotions such as fear • Seborrheic dermatitis – causes
(“cold sweat”) scaly, flaky, itchy patches over
sebum-rich areas of the skin of
• Mammary Glands Found only in the scalp, face, and occasionally
mammals. Are structurally related to the trunk of the body (e.g.,
the skin in that they are a modified type dandruff, “cradle cap” in
of sweat gland but functionally related infants)
to the reproductive system because • Unknown cause but
they produce milk to nourish offspring. thought to be caused
by a fungal infection
• Endocrine glands, which
• Condition can become
release secretions directly into the bloodstream or
chronic in individuals
tissue spaces to be circulated throughout the body
with decreased
Nerve Endings immunity
• Atopic dermatitis (eczema) –
- Also called “receptors,” the skin contains chronic rash and dry, thickened
millions of them all over the body skin
- Located in the dermis Treatments for atopic dermatitis:
- The sensitivity of an area of skin is related to • Oral drugs to control symptoms
the number of receptors present, making some and spread (antihistamines and antibiotics)
areas more sensitive than others • Phototherapy: Exposure to
- Send nerve impulses to the brain when they ultraviolet (UV) light, which can kill certain
detect changes (pain, heat, cold, etc.) cells involved in skin disease
– Sometimes combined • Invades skin to deep dermis and
with psoralen, a drug taken orally before spreads quickly, resulting in redness, swelling,
treatment to lessen effects of UV therapy and tenderness
– PUVA (POO-va) • Peau d’orange: Term used to
therapy: An acronym for the oral describe tense skin resembling the peel of an
administration of psoralen and UV light orange
• Topical immunomodulators • Diagnosis made by skin
(TIMs): Drugs that inhibit inflammatory skin appearance as well as blood cultures and/or
reactions (Protopic, Elidel) skin biopsies.
• Rosacea: a chronic skin • Complications of cellulitis
condition causing redness and flushing around the • Strep cells can invade the body
center of the face and eyes and result in:
- Cause unknown, but thought to be hereditary • Cardiac impairment (bacterial
• Treatments for rosacea endocarditis), an infection of the heart
• Topical antibiotics muscle
(metronidazole and clindamycin) to improve • Infections of the lymph nodes
health and appearance of the skin throughout the body
• Oral antibiotics (tetracycline, • Gangrene (tissue death) and
doxycycline, erythromycin) flesh-eating bacteria
• Electrosurgery and laser • Treatments:
surgery to reduce the visibility of blood vessels • Antibiotic treatments
in the face and improve facial appearance (penicillin)
• Psoriasis: A chronic disease characterized by • Cool, wet dressings to infected
red, raised patches with silvery scales (plaques) due skin
to an abnormally high rate of skin cells. Cause is • Impetigo
unknown. – A contagious skin infection leading to
• Treatments for psoriasis: fluid-filled, honey-colored clusters called bullae on
• Treatment to reduce the growth of skin the body
cells (Dovonex ointment) – Commonly affects children and is
• Phototherapy and PUVA therapy spread by fluid that oozes from the blisters
• Exposure to natural sunlight – Caused primarily by Streptococcus or
Staphylococcus aureus, or a combination of both
Skin Infections – Treatments
• Skin infections occur when skin barrier is broken – Antibiotic ointments (Bactroban)
and bacteria, viruses, fungi, and parasites enter – Oral antibiotics for more severe cases
the body (dicloxacillin, erythromycin, or
• Three most common types: cephalexin) to clear the lesions.
– Bacterial • Folliculitis
– Fungal – a bacterial infection of hair follicles that develops
– Viral when bacteria (most commonly Staphylococcus aureus)
Bacterial Skin Infections invades the skin
– Cellulitis: an acute bacterial infection of – Boil: A warm, painful, pus-filled pocket
the skin and underlying tissues of infection below the skin’s surface
• Most common bacterial cause: – Carbuncle: A cluster of abscesses
Streptococcus species connected to each other under the skin
– Treatments
– Topical antibiotic creams (neomycin, • Antifungal creams (nystatin or
bacitracin) clotrimazole creams) applied to the affected
– Oral antibiotics to kill staphylococci area
• Oral antifungal drugs (fluconazole) to be
taken internally
Fungal Skin Infections
• Caused by dermatophytes (microscopic
organisms) that live on keratin in skin Viral Skin Infections
• Warmth, moisture, or irritation to the skin can • Caused by a virus entering the skin and causing
cause them to grow uncontrollably, resulting in skin conditions requiring treatment by a
a skin infection physician
• Mycosis: Another name for “fungal infection of • Warts
the skin” - also called verrucae, are small skin growths caused
• Mycologist: A person who identifies and by the Papillomavirus
classifies fungal infections • Plantar warts—bottom of the foot
• Filiform warts—face, neck, or lips
• Tinea • Genital warts—around the genitals;
- another name for ringworm, because of the circular also called condyloma acuminata
shape of the rash • Verrucae vulgaris—on the hands, arms,
• Tinea capitis—scalp or neck and legs; also called common warts
• Tinea barbae—beard area • Treatments:
• Tinea corporis—nonhair parts of the • Often go away on their own
body (arms, shoulders, and face) • Over-the-counter corrosive agents
• Tinea cruris—groin, also called jock itch • Surgically removed with cryotherapy
• Tinea pedis—feet, also called athlete’s (freezing), electrocautery (burning), or
foot laser surgery
• Treatment for ringworm: • Shingles
• The use of special shampoo to eliminate - also called herpes zoster
fungus on the scalp • A viral infection of the nerves caused by
• Oral antifungal medication or steroids reactivation of the varicella-zoster virus that
to help destroy the fungus and reduce causes chickenpox
inflammation of the skin • “Chickenpox” initial manifestation of
• Candidiasis the virus, which re-emerges after laying
- commonly called a fungal infection, yeast infection, dormant in the spinal or cranial nerves for
or thrush several years, causing pain and a painful
- Caused by the Candida species of fungi rash on the skin
- Candida: small, thin-walled yeasts that reproduce • Chronic pain that remains in the area
by budding after rash is called postherpetic neuralgia
- Candida albicans: probably the most common form • Treatments
of skin disease in humans • Topical creams (sulfadiazine)
- Cutaneous candidiasis: infection of the skin with • Oral antivirals (acyclovir, famciclovir,
Candida, the most common form of candidiasis valacyclovir)
(intertrigo and diaper rash are common Damage from Heat and Cold
manifestations) • Burn
• Treatments for candidiasis
– an injury caused by heat, electricity, chemicals, or – Split-thickness skin graft: a graft that
radiation includes the epidermal layer and part of
– Destroys layers of skin the dermal skin layers
– May require long-term medical care, – Full-thickness skin graft: consists of
multiple surgeries, and psychological treatment both the epidermal and complete
• First degree dermal skin layers
– Outer layer (epidermal) of skin – Artificial skin grafts: skin substitutes
– No blisters created in the laboratory that contain
– Heal quickly components of donated skin tissue that
• Second degree is more useful because it will not be
– Affects both epidermal and rejected by the body
dermal layers • Frostbite
– Burns heal but leave a change - an injury to skin and underlying tissues resulting
in skin color from exposure to very cold temperatures
• Third degree – Ice crystals begin to form in the tissues
– Destroys all the epidermal and dermal – Ice crystals cause the skin to rupture,
skin layers killing skin cells
– Damage extends to deep subcutaneous • First degree
tissue – Temporary tenderness and numb
– The skin becomes charred and leathery – White patches of skin that peel after
• Fourth degree warming
– Deep enough to involve muscle, bone, – No permanent skin damage
tendon, and/or ligaments • Second degree
– Life-threatening – Formation of blisters
• Burn Treatments – Underlying tissue is unharmed
– Topical antibiotic cream for minor burns • Third degree
– Debridement: dead tissue and debris – Extremity feels cold, numb, and hard
are removed from wound to expose – Underlying tissue damage that feels
and cleanse the area hard and cold
• Dressings: materials used to – Eventually requires skin grafts or
cover and protect the wound amputation of the affected limb
• Dressing changes: the process Skin Cancers
of removing old bandages and • The most common form of cancer in the U.S.
replacing them with new ones • Ultraviolet radiation is the main cause of skin
• Skin Grafting cancer
- where a layer of healthy skin is taken from another • Develop when DNA in skin tissues becomes
area of the body and transferred to the area of skin damaged and the body cannot repair the
defect damage. Damaged cells multiply and divide
– Autologous graft (autograft): graft uncontrollably, forming a mass, called a lesion
taken from the patient’s own skin or tumor, on the skin.
– Cadaver graft (allograft): graft taken • Most skin cancers detectable and treatable at
from the skin of a dead person an early stage
– The graft is applied and takes up blood • Three main types, named after the type of cell
supply from the wound, helping it to survive in which it originates: basal cell, squamous cell,
• Types of Grafts: and melanoma
• Basal cell carcinoma
– Most common skin cancer – Punch biopsy: removal of a cylinder of
– Begin in the basal cells located in the skin with a sharp, punchlike instrument
lowest layer of the epidermis – Excisional biopsy: removal of the entire
– Generally do not spread to other parts lesion for analysis
of the body • KOH test (pronounced K-O-H)
• Squamous cell carcinoma – A microscopic examination of skin, hair,
• Begins in the squamous cells located in or nails for the presence of fungus
the upper levels of the epidermis – Named after potassium hydroxide
• Can spread to other parts of the body (KOH), which is used to help identify
• Melanoma fungi in the sample
• Arises from the melanocytes in the • Tzanck Test
epidermis – Also called “herpes skin test” or
• Most harmful; prognosis poor if not “chickenpox skin test”
caught early – Tests for herpes simplex virus, which
• ABCD method for evaluating suspicious causes cold sores, fever blisters, or
skin lesions: genital sores
• A: Asymmetry – uneven or – Also tests for presence of varicella
irregular shape zoster virus (for chickenpox and
• B: Border irregularity – smooth shingles)
or jagged or notched
• C: Color variation – various
colors may indicate skin cancer
• D: Diameter of 6 mm or more
– cancerous lesions grow larger than regular
moles
• Treatments
– Curettage and desiccation
• Curettage: removing the lesion with a
scooplike instrument called a curette
• Desiccation: application of electric
current to the area to control bleeding
and kill remaining cancer cells
– Surgical excision
– Radiation therapy: high-energy x-rays kill or
shrink cancer cells
– Cryosurgery: freeze and kill abnormal cells
– Mohs surgery: process of removing tumor layer
by layer
- Chemotherapy for malignant melanoma
Diagnostic Studies and Procedures
• Skin Biopsy: removing a sample of skin and
examining it under a microscope
– Shave biopsy: removes only superficial
levels of skin
You might also like
- Expository Writing ModuleDocument30 pagesExpository Writing ModulePau De Guzman38% (8)
- The Case of George EthicsDocument4 pagesThe Case of George EthicsPau De GuzmanNo ratings yet
- M1 Pre-Task: The Trolley ProblemDocument20 pagesM1 Pre-Task: The Trolley ProblemPau De Guzman75% (4)
- M3 Lesson 1: Reason and Impartiality - While Task 1: Case Study: What Should We Do?Document3 pagesM3 Lesson 1: Reason and Impartiality - While Task 1: Case Study: What Should We Do?Pau De Guzman100% (1)
- Pulmonology - Study Guide PDFDocument77 pagesPulmonology - Study Guide PDFDanielle Groupfive100% (2)
- Module 3 Skinbody MemranesDocument3 pagesModule 3 Skinbody MemranesRaphael SevillaNo ratings yet
- Integumentary & Skeletal SystemDocument4 pagesIntegumentary & Skeletal SystemMaisonette MichNo ratings yet
- Integumentary SystemDocument2 pagesIntegumentary SystemALEXIS MOIRAH CALIGAGANNo ratings yet
- Corneum and Is Directly Exposed To TheDocument3 pagesCorneum and Is Directly Exposed To Theydnic alykPNo ratings yet
- Integumentary SystemDocument3 pagesIntegumentary SystemCarmela Cordon FelixNo ratings yet
- Cells Are Scattered Around: Pigment That Affords The Skin Some Protection Against Ultraviolet RadiationDocument5 pagesCells Are Scattered Around: Pigment That Affords The Skin Some Protection Against Ultraviolet RadiationDimple Lexiry GloriaNo ratings yet
- 5 Integumentary SystemDocument5 pages5 Integumentary SystemEly FructuosoNo ratings yet
- Chap3 Integ Anaphy NotesDocument11 pagesChap3 Integ Anaphy NotesAxel Neil VidalNo ratings yet
- MC 1 Lecture (Anatomy & Physiology) Chapter 4Document4 pagesMC 1 Lecture (Anatomy & Physiology) Chapter 4Cinderilla De AngelNo ratings yet
- Integumentary SystemDocument54 pagesIntegumentary SystemKhaela Mercader100% (2)
- Lecture 1Document30 pagesLecture 1Dr. Rabail MalikNo ratings yet
- PowerPoint - Presentation - About - Integumentary - SystemDocument27 pagesPowerPoint - Presentation - About - Integumentary - SystemPrayl Hope NapanoNo ratings yet
- Integumentary SystemDocument4 pagesIntegumentary SystemOddysa EstorqueNo ratings yet
- Anatomy 3-4Document13 pagesAnatomy 3-4Gladys Mae S. BañesNo ratings yet
- Anatomy & Physiology Reviewer: Stratum GerminativumDocument5 pagesAnatomy & Physiology Reviewer: Stratum GerminativumChris Deinielle Marcoleta SumaoangNo ratings yet
- MOYA, John Zeus A. (HUMANA Classwork #3 Prelim)Document41 pagesMOYA, John Zeus A. (HUMANA Classwork #3 Prelim)Suez AyomNo ratings yet
- Skin Physiology: Lecturer:Dr Herman Mulijadi MS, SPKPDocument59 pagesSkin Physiology: Lecturer:Dr Herman Mulijadi MS, SPKPJosephine SNo ratings yet
- Integumentary SystemDocument18 pagesIntegumentary SystemRenjyl Gay DeguinionNo ratings yet
- Integumentary SystemDocument8 pagesIntegumentary SystemreinajoannaNo ratings yet
- MC1 REVIEWER (Integumentary System)Document7 pagesMC1 REVIEWER (Integumentary System)Francine Dominique CollantesNo ratings yet
- Integumentary SystemDocument5 pagesIntegumentary SystemChan TalNo ratings yet
- Integumentary System 1Document12 pagesIntegumentary System 1Akemi LeeNo ratings yet
- I) Skin Largest Organ of The Body in Surface Area and Weight. There Are Three Layers of The Skin 1. Epidermis 2. Dermis 3. Subcutaneous TissueDocument44 pagesI) Skin Largest Organ of The Body in Surface Area and Weight. There Are Three Layers of The Skin 1. Epidermis 2. Dermis 3. Subcutaneous TissueSaralitaNo ratings yet
- Skin & MembraneDocument8 pagesSkin & MembraneLeigh Andrei Dela CruzNo ratings yet
- The Integumentary System: (Anatomy of The Skin, Hair, and Nails)Document3 pagesThe Integumentary System: (Anatomy of The Skin, Hair, and Nails)Venus Amoroso BaguiosoNo ratings yet
- AP 5 Integumentary SystemDocument120 pagesAP 5 Integumentary SystemIkhsan HidayatNo ratings yet
- Integumentary SystemDocument6 pagesIntegumentary Systemericamaeabellanosa22No ratings yet
- Integumentary System ANAPHY Notes 4Document5 pagesIntegumentary System ANAPHY Notes 4Alloiza CaguiclaNo ratings yet
- Anaphy ReviewerDocument8 pagesAnaphy ReviewerMark GonzalesNo ratings yet
- Zoology Lecture (Reviewer)Document4 pagesZoology Lecture (Reviewer)Maria GrasyaNo ratings yet
- Chapter 5 ANAPHY The Integumentary SystemDocument2 pagesChapter 5 ANAPHY The Integumentary Systemrobh0026No ratings yet
- Chap5 - Integument TransesDocument4 pagesChap5 - Integument TransesSophia Margarette CawalingNo ratings yet
- Integumentary System, EdDocument42 pagesIntegumentary System, EdGirmay GebrehiwotNo ratings yet
- Anaphy Topic 3 IntegralDocument3 pagesAnaphy Topic 3 Integral박제라No ratings yet
- Integumentary SystemDocument9 pagesIntegumentary SystemBeah Marie AlisosoNo ratings yet
- Integumentary System PDF 2Document8 pagesIntegumentary System PDF 2thyezlianNo ratings yet
- What Is The Integumentary System?Document6 pagesWhat Is The Integumentary System?Jerneth Nyka FloresNo ratings yet
- S4 Integumentary SystemDocument9 pagesS4 Integumentary Systemcam broquelNo ratings yet
- Microscopic Analysis of The Integumentary SystemDocument9 pagesMicroscopic Analysis of The Integumentary SystemAgatha joy MadrazoNo ratings yet
- Integumentary SystemDocument6 pagesIntegumentary SystemwannabeeurzNo ratings yet
- Nursing AnaPhy Integumentary SystemDocument22 pagesNursing AnaPhy Integumentary SystemGail Chantel Spring PerlasNo ratings yet
- Anatomy & Physiology With Pathophysiology Lecture (Midterms)Document4 pagesAnatomy & Physiology With Pathophysiology Lecture (Midterms)Millen ArenasNo ratings yet
- Biol163 Integumentary SystemDocument46 pagesBiol163 Integumentary SystemGladdyll Raico DizonNo ratings yet
- 10 Integumentary SystemjjjDocument51 pages10 Integumentary SystemjjjjkkjkjjkNo ratings yet
- Integumentary System: Dr. Ammarah NaseerDocument67 pagesIntegumentary System: Dr. Ammarah NaseerAaqib RiazNo ratings yet
- Integumentary SystemDocument9 pagesIntegumentary SystemCelyn DeañoNo ratings yet
- WEEK 5 TRANS AnaphyDocument2 pagesWEEK 5 TRANS AnaphygazzyngsalvadorNo ratings yet
- Skin and Appendages (PFOS-1 2014-15 Students Version)Document24 pagesSkin and Appendages (PFOS-1 2014-15 Students Version)Chris Jardine LiNo ratings yet
- Angee 11Document4 pagesAngee 11lunadawsonesNo ratings yet
- Physiology of SkinDocument29 pagesPhysiology of SkinIlham KurniawanNo ratings yet
- 176 Anatomy Integumentary SystemDocument29 pages176 Anatomy Integumentary SystemJoana Mae PortezaNo ratings yet
- Anaphy Lec Midterm ReviewerDocument27 pagesAnaphy Lec Midterm ReviewerFAITH EFONDONo ratings yet
- Introduction To Dermatology: Marwa El-SamongyDocument16 pagesIntroduction To Dermatology: Marwa El-SamongyAbdalla esayedNo ratings yet
- Integumentary System ReviewerDocument5 pagesIntegumentary System ReviewerFayena JoseNo ratings yet
- Chapter 5 - Integumentary SystemDocument5 pagesChapter 5 - Integumentary SystemLora Mae Delos SantosNo ratings yet
- Anaphy - IntegumentaryDocument4 pagesAnaphy - IntegumentaryYo1No ratings yet
- 5 - IntegDocument8 pages5 - IntegGel Austin PascuaNo ratings yet
- Chapter 5 Anatomy and PhysiologyDocument7 pagesChapter 5 Anatomy and PhysiologyAngela Mae MeriñoNo ratings yet
- Histom 8 9 10Document5 pagesHistom 8 9 10Jehira OcampoNo ratings yet
- M4 Post-TaskDocument2 pagesM4 Post-TaskPau De GuzmanNo ratings yet
- Situation A:: M5 Lesson 1: Theories of Justice - While Task 1Document2 pagesSituation A:: M5 Lesson 1: Theories of Justice - While Task 1Pau De Guzman100% (1)
- Reading Material - Skeletal SystemDocument38 pagesReading Material - Skeletal SystemPau De GuzmanNo ratings yet
- Process of Writing For Non-Writers - PPSXDocument53 pagesProcess of Writing For Non-Writers - PPSXPau De GuzmanNo ratings yet
- Subject Title: Medical Technology vs. Coronavirus Pre-Writing Who?Document2 pagesSubject Title: Medical Technology vs. Coronavirus Pre-Writing Who?Pau De GuzmanNo ratings yet
- BSMT2C DE GUZMAN OutlineDocument1 pageBSMT2C DE GUZMAN OutlinePau De GuzmanNo ratings yet
- General Surgery ConceptsDocument4 pagesGeneral Surgery ConceptsPau De GuzmanNo ratings yet
- Blood Tests & Normal RangeDocument40 pagesBlood Tests & Normal RangeSuria KumarNo ratings yet
- L2 Integumentary Assessment PDFDocument46 pagesL2 Integumentary Assessment PDFElizabeth AbellaNo ratings yet
- Chapter 15 Lung Pathology ErnieDocument20 pagesChapter 15 Lung Pathology ErnieZandra Lyn AlundayNo ratings yet
- Obgyn: History Taking and Examination DR Musa Marena ObgynDocument94 pagesObgyn: History Taking and Examination DR Musa Marena ObgynnidoNo ratings yet
- Acute Myeloid Leukemia With Myelodysplasia RelatedDocument6 pagesAcute Myeloid Leukemia With Myelodysplasia RelatedAgus WiniNo ratings yet
- 02 Mar 2021 PDFDocument8 pages02 Mar 2021 PDFVaibhav RamNo ratings yet
- Galea - Abdominal Pain in ChildhoodDocument30 pagesGalea - Abdominal Pain in Childhoodsanty anggroiniNo ratings yet
- Herliani, Abrani Sulaiman, M. Ilmi Hidayat: Penulis Koresponden: Herliani@ulm - Ac.idDocument5 pagesHerliani, Abrani Sulaiman, M. Ilmi Hidayat: Penulis Koresponden: Herliani@ulm - Ac.idTarisya I.W 18.3151No ratings yet
- Adjuvant Icotinib Versus Observation in Patients WDocument11 pagesAdjuvant Icotinib Versus Observation in Patients WVanilson BorgesNo ratings yet
- ReferenceDocument7 pagesReferenceAshley CesaNo ratings yet
- Acute Viral Syndrome: Case Presentation OnDocument22 pagesAcute Viral Syndrome: Case Presentation OnSafoora RafeeqNo ratings yet
- Renal Replacement TherapyDocument23 pagesRenal Replacement TherapybgfhnfgNo ratings yet
- The Diagnosis of Organic Brain Syndrome: TfcqtureDocument4 pagesThe Diagnosis of Organic Brain Syndrome: TfcqtureWonderCatNo ratings yet
- Gi DisordersDocument53 pagesGi DisordersJulie EstebanNo ratings yet
- Anaphylaxis Guidelines PosterDocument1 pageAnaphylaxis Guidelines PosterBabo SanNo ratings yet
- Alcoholic Hepatitis Diagnosis and ManagementDocument10 pagesAlcoholic Hepatitis Diagnosis and ManagementGW GeistNo ratings yet
- 23 Cervix Uteri Fact Sheet PDFDocument2 pages23 Cervix Uteri Fact Sheet PDFIrina DeaconescuNo ratings yet
- Physio After SurgeryDocument2 pagesPhysio After SurgeryGursangeet KaurNo ratings yet
- Online VIREAD Tenofovir Disoproxil Fumarate Purchase With DiscountDocument5 pagesOnline VIREAD Tenofovir Disoproxil Fumarate Purchase With Discountcena heyNo ratings yet
- Reflexology: Presented by Megan ReidDocument14 pagesReflexology: Presented by Megan ReidHendi Prayuda WidodoNo ratings yet
- ANC and BFDocument29 pagesANC and BFRose Anne Tusi BotinNo ratings yet
- Heart Disease and Stroke BrochureDocument3 pagesHeart Disease and Stroke Brochureapi-461951012No ratings yet
- Acute Kidney Injury PosterDocument1 pageAcute Kidney Injury Postermmbire@gmail.comNo ratings yet
- CHF Literature ReviewDocument5 pagesCHF Literature Reviewapi-509632460No ratings yet
- Biology Viral DiseasesDocument11 pagesBiology Viral DiseasesPrasoon Singh RajputNo ratings yet
- The Effects of A Shoulder Roll During LaryngosDocument11 pagesThe Effects of A Shoulder Roll During LaryngospaulaNo ratings yet
- DRUG-STUDY - CelecoxibDocument3 pagesDRUG-STUDY - Celecoxibamal abdulrahmanNo ratings yet
- Epidemiology of Ocular Tumors 2013Document230 pagesEpidemiology of Ocular Tumors 2013Ranny LaidasuriNo ratings yet
- Paper AnalysisDocument4 pagesPaper AnalysisLayali MassisNo ratings yet