Professional Documents
Culture Documents
IV Anaesthetics Spreadsheet
Uploaded by
DonkeyManOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
IV Anaesthetics Spreadsheet
Uploaded by
DonkeyManCopyright:
Available Formats
Table compiled by
B.J. So, Feb 2018 Propofol Thiopentone Ketamine Etomidate Midazolam
Structure and
class1,4
Pharmaceutics
2,6-diisopropylphenol Thiobarbiturate Phencyclidine derivative Carboxylated imidazole derivative Imidazobenzodiazepine
(a phenol derivative)
1% propofol emulsion with: Yellow powder stored with 6% Na2CO3 Clear colourless solution (typically 10mg/ml) Original: clear colourless solution with 35%
10% soybean oil Clear colourless solution with pH 3.5
propylene glycol (pH 6.9)
Distinguishing 2.25% glycerol 500mg reconstituted in 20ml water = 2.5% solution (mostly ring open; protonated)
pH 3.5-5.5
pharmaceutic 1.2% purified egg phosphatide (pH 10.5 to prevent microcrystal formation)
Later: lipid emulsion (pH 7.6)
features Sodium hydroxide Demonstrates tautomerism with open (acidic) and
Racemic mixture: Racemic mixture:
closed (basic) ring forms
Neutral pH 7.4 S- enantiomer more potent at GABAA S(+) has x4 greater affinity for NMDA receptor Enantiopure in the R(+) form
PK: A
Absorption4 N/A N/A 25% (PO), 50% (nasal), 93% (IM) N/A 50% (PO)
pKa1 11.0 (acid) 7.6 (acid) 7.5 (base) pKa 4.2 (base) pKa 6.15 (base)
% non-ionised at
99.7% 61% 44% 99% 90% (ring open; unprotonated)
pH 7.43
PK: D
Protein binding1 98% (very highly bound) 1,4 80% (highly bound) 20% (minimally bound) 75% (highly bound) 98% (very highly bound)
VDss4 4 L/kg 2 L/kg 3 L/kg 4 L/kg1 1 L/kg1
Follows a 3-compartment model Follows 3-compartment model x5-10 more lipid soluble than thiopentone Follows 2 or 3 compartment model Follows 2 compartment model
Comments Offset of clinical effects mainly due to distribution Offset of clinical effects mainly due to distribution Offset of clinical effects mainly due to distribution Offset of clinical effects mainly due to distribution Offset of clinical effects mainly due to distribution
60%: CYP2B6 hydroxylation +
P450 oxidation in liver with low hepatic extraction Hydrolysis by CYP3A4 into active and inactive
glucuronidation and sulfation in liver with high ER Demethylation and hydroxylation in liver
coefficient (15%) ∴ clearance is capacity-limited
PK: M
1 ∴ clearance is flow-dependent Hydrolysis by hepatic and plasma esterases into metabolites.
Metabolism
Zero-order kinetics at high concentrations inactive metabolites
40%: Extra-hepatic metabolism in kidney + small Norketamine metabolite ~25% potency
(Michaelis–Menten elimination) 1-hydromidazolam has 50% potency
intestine
Elimination half-life 0.5 – 1.5 hours3
PK: E
Excretion4 Elimination half-life 3-22 hours4 Elimination half-life 2-3 hours3 Elimination half-life 2-5 hours3 Elimination half-life 2 hours3
CSHT after 8-hour infusion: <40 mins3
Typical Dose 2mg/kg 5mg/kg 1-2mg/kg 0.3mg/kg
0.3 mg/kg1
(range) (1.5-2.5mg/kg) (2-7mg/kg) (0.2-0.5mg/kg for analgesia) (0.2-0.4 mg/kg)
PD: D
Onset1 1 minute2,4 1 minute1 1 minute2 1 minute4 2 minutes1
Duration1 5-10 minutes2 3-7 minutes1 10-15 mins, with ~60 min amnesia3 6-10 minutes4 20 minutes1
(or 4.5 hours after 3-day infusion)
Potentiates GABAA receptor activity Non-competitive antagonist of NMDA
PD: M
Mechanism3 Potentiates GABAA receptor activity (allosteric binding causing ↑GABA affinity) Potentiates GABAA receptor activity Potentiates GABAA receptor activity
(decreases rate of GABA dissociation from receptor)3
receptor (enhances affinity of GABA at receptor)3 (allosteric binding causing ↑GABA affinity)3
*Can directly act on GABAA receptors at high dose* (acts on phencyclidine binding site)
↓CBF, ↓ICP, ↓CMRO2 ↓CBF, ↓ICP, ↓CMRO2 ↑CBF, ↑ICP, ↑CMRO2 ↓CBF, ↓ICP, ↓CMRO2 ↓CBF, ↓ICP, ↓CMRO2
CNS1,3,4 Anticonvulsant Anticonvulsant Anticonvulsant Epileptogenic Anticonvulsant
↓IOP ↓IOP ↑IOP ↓IOP ↓IOP
Potent depressant (*depresses baroreceptor reflex) Mild CVS depressant CVS stimulant + ↑myocardial O2 demand Relatively CVS neutral Mild CVS depressant
CVS1,3,4 (↓contractility, ↓↓SVR, ↓HR*) (↓contractility, ↓SVR, but ↑HR) (↑contractility, ↑HR, but ↔SVR) (MAP, HR, SVR unchanged) (↓contractility, but ↔SVR and ↑HR)
Potent respiratory depressant Potent respiratory depressant No respiratory stimulation/depression
Minimal respiratory depression
Resp1,3,4 Supresses laryngeal reflexes Can cause laryngospasm Preserves airway reflexes + ↑secretions Respiratory depressant
Associated with hiccupping
PD: E
Causes bronchodilation Can cause bronchoconstriction Effective bronchodilator
Painless if given IV Painful in original form
Irritation1,3,4 Pain on injection None None
Highly irritant if extravasates due to alkalinity Painless in lipid emulsion form
“Dissociative anaesthesia” Contraindicated in porphyria
Antiemetic (EEG dissociation between thalamocortical Contraindicated in porphyria
Antipruritic and limbic systems)
Inhibits adrenal steroidogenesis
Contraindicated in porphyria ↓PONV
Other1,3,4 Propofol infusion syndrome ↑PONV ↑PONV
Enzyme inducer Can inhibit platelet aggregation
(in large prolonged doses: metabolic acidosis, Can inhibit platelet aggregation Can inhibit platelet aggregation
rhabdomyolysis, multi-organ failure)
Prolonged use can lead to withdrawal in paeds
Risk of emergence delirium Associated with myoclonic jerks
Sources: 1 Evers Anesthetic Pharmacology 2nd ed., chapter 27-28 / 2 Miller’s Anesthesia 8th ed., chapter 30/ 3 Stoelting Pharmacology and Physiology in Anesthesia 5th ed., chapter 5 / 4 Oxford Handbook of Drugs 5th edition / 5 Peck and Hill Pharmacology 4th edition chapter 9
You might also like
- TANNIN - Resin - FlavanoidDocument44 pagesTANNIN - Resin - FlavanoidParajapati SanjivNo ratings yet
- Chapter 1 - Introduction To Petroleum ChemistryDocument14 pagesChapter 1 - Introduction To Petroleum ChemistryPrincessFaraBP100% (1)
- Physical Science Exam PDFDocument2 pagesPhysical Science Exam PDFRemar Jhon PaineNo ratings yet
- Monsanto Experiment 5 Amino AcidsDocument6 pagesMonsanto Experiment 5 Amino AcidsRhey Christian MonsantoNo ratings yet
- Module 3 Electrons in AtomsDocument23 pagesModule 3 Electrons in AtomsJulie Anne Manggurit (Grade-10 Tesla)No ratings yet
- Antiseptics Disinfectants For Veterinary UseDocument22 pagesAntiseptics Disinfectants For Veterinary UseSunil100% (5)
- Acid-Base Indicators Ph-Range PDFDocument3 pagesAcid-Base Indicators Ph-Range PDFformoviejuneNo ratings yet
- Clariant Brochure Methanol Synthesis 201711 ENDocument16 pagesClariant Brochure Methanol Synthesis 201711 ENCrystal DaiNo ratings yet
- Vda 232-101 Gadsl Global Automotive Declarabe Substance ListDocument44 pagesVda 232-101 Gadsl Global Automotive Declarabe Substance ListAugusto Kuribara100% (1)
- Proposal Sample PDFDocument79 pagesProposal Sample PDFIgnatius Matthew DabucoNo ratings yet
- Base Oil - Pertamina PDFDocument52 pagesBase Oil - Pertamina PDFspurwito46No ratings yet
- Essential Oils in Food Processing: Chemistry, Safety and ApplicationsFrom EverandEssential Oils in Food Processing: Chemistry, Safety and ApplicationsSeyed Mohammed Bagher HashemiNo ratings yet
- Inventaris Limbah B3Document40 pagesInventaris Limbah B3Echa Luph Khansa Amin100% (2)
- IV Anaesthetics SpreadsheetDocument2 pagesIV Anaesthetics SpreadsheetDonkeyManNo ratings yet
- Classification of LipidsDocument7 pagesClassification of LipidsBreanne Pearl Angelie DumbriqueNo ratings yet
- PH Water On Stability PesticidesDocument6 pagesPH Water On Stability PesticidesMontoya AlidNo ratings yet
- Experiment No. 5: Amino AcidsDocument6 pagesExperiment No. 5: Amino AcidsAna LuisaNo ratings yet
- The Optimum Conditions For Production of Soya Peptone by Acidic Hydrolysis of Soya ProteinsDocument19 pagesThe Optimum Conditions For Production of Soya Peptone by Acidic Hydrolysis of Soya ProteinsLenny SandyNo ratings yet
- 192 12 56 14 TegosoftGCDocument9 pages192 12 56 14 TegosoftGCAhmed elsayehNo ratings yet
- Summary of Common Opioids: Opioid Morphine Oxycodone Fentanyl Alfentanil Remifentanil PethidineDocument2 pagesSummary of Common Opioids: Opioid Morphine Oxycodone Fentanyl Alfentanil Remifentanil PethidineSammuel1324No ratings yet
- Dermosoft 1388 ECO. Product Info. 04.01.19Document6 pagesDermosoft 1388 ECO. Product Info. 04.01.19sairaNo ratings yet
- Intro To Drug & Dosage Form DesignDocument74 pagesIntro To Drug & Dosage Form DesignAbhiraj KawadeNo ratings yet
- Experiment 1 & 2 Habitan, Sheena Joy C. 2Bsph1 08/24/21Document4 pagesExperiment 1 & 2 Habitan, Sheena Joy C. 2Bsph1 08/24/21SHEENA JOY HABITANNo ratings yet
- Bunge-Enzymatic Degumming For PRDocument23 pagesBunge-Enzymatic Degumming For PRarcenioNo ratings yet
- Hair Protection SprayDocument1 pageHair Protection SprayCinthia GómezNo ratings yet
- Evolution of Muguet Accords 1926 1932 1949 1960 1970 1980 Synonyms/NotesDocument1 pageEvolution of Muguet Accords 1926 1932 1949 1960 1970 1980 Synonyms/Notesarandes62No ratings yet
- Fda Minimum Requirement For Analysis of Fnished Product Annex JDocument21 pagesFda Minimum Requirement For Analysis of Fnished Product Annex JCarlo TierraNo ratings yet
- Separation of Salicylic Acid Impurities With DiffeDocument4 pagesSeparation of Salicylic Acid Impurities With Diffemic92833292No ratings yet
- 04 - PA Perkebunan-DikonversiDocument54 pages04 - PA Perkebunan-DikonversiCinthia Syafira DarmawanNo ratings yet
- Summary of Qualitative Tests (Pharmacognosy)Document8 pagesSummary of Qualitative Tests (Pharmacognosy)kidsaintfineNo ratings yet
- ResponsiDocument8 pagesResponsioliviaNo ratings yet
- Black Tea SpecDocument34 pagesBlack Tea SpecImmakulata CindyNo ratings yet
- Academic SciencesDocument6 pagesAcademic SciencesUrva VasavadaNo ratings yet
- Bio-Based Polymers in The WorldDocument35 pagesBio-Based Polymers in The WorldCarlotta C.No ratings yet
- We 10-12Document1 pageWe 10-12Oula HatahetNo ratings yet
- We 10-12Document1 pageWe 10-12Oula HatahetNo ratings yet
- 4 - Caffeine ExtractionDocument1 page4 - Caffeine ExtractionTien NguyenNo ratings yet
- Water Treatment PlantDocument15 pagesWater Treatment PlantBhaskar BethiNo ratings yet
- Emulsi Olive OilDocument5 pagesEmulsi Olive OilCut RifqaNo ratings yet
- Determinación de Parabenos Por HPLCDocument5 pagesDeterminación de Parabenos Por HPLCVanessa Vigo AyvarNo ratings yet
- A - Lúpulo Ahhhroma PelletsDocument1 pageA - Lúpulo Ahhhroma PelletsWindson InativoNo ratings yet
- 4468-Article Text-9902-1-10-20180301Document12 pages4468-Article Text-9902-1-10-20180301Firda ZuliatulNo ratings yet
- Universitas Muhammadiyah Prof - Dr.hamka Sulistiani 193 1 Jurnals IDocument11 pagesUniversitas Muhammadiyah Prof - Dr.hamka Sulistiani 193 1 Jurnals IDewiAndrianiKhanajmiNo ratings yet
- Bioprox 100whey Protein Concentrate PDFDocument1 pageBioprox 100whey Protein Concentrate PDFPABLONo ratings yet
- Effect of Water PH On The Stability of Pesticides - MSU ExtensionDocument6 pagesEffect of Water PH On The Stability of Pesticides - MSU ExtensionWahyudiNo ratings yet
- Chemistry Practical Report: Date of Submission Received by Score 5th March 2018Document10 pagesChemistry Practical Report: Date of Submission Received by Score 5th March 2018prettyNo ratings yet
- Pharmaceutics and ChemistryDocument12 pagesPharmaceutics and Chemistryyoussef.koko1212No ratings yet
- Chemical Compatibility ChartDocument1 pageChemical Compatibility ChartVinit Kumar MishraNo ratings yet
- Gabatin, Bea B. - Introduction To Organic AgricultureDocument13 pagesGabatin, Bea B. - Introduction To Organic Agriculturebeabaldomero18No ratings yet
- Appendix Vii Part 5Document3 pagesAppendix Vii Part 5cosmpiroNo ratings yet
- Results and Discussionexp1Document4 pagesResults and Discussionexp1Vince PaelmoNo ratings yet
- Shell Rubber Untuk CPO Diaktivasi KOHDocument7 pagesShell Rubber Untuk CPO Diaktivasi KOHHilmi FebrianNo ratings yet
- 20150527123031e Coconut Oil Virgin CofA 240415-4Document2 pages20150527123031e Coconut Oil Virgin CofA 240415-4azarine wahanaNo ratings yet
- Preparation of BakeliteDocument8 pagesPreparation of Bakeliteusman_uet0868% (19)
- Effects of Various Liquid Organic Solvents On Solvent-Induced Crystallization of Amorphous Poly (Lactic Acid) FilmDocument11 pagesEffects of Various Liquid Organic Solvents On Solvent-Induced Crystallization of Amorphous Poly (Lactic Acid) FilmqueteimportaNo ratings yet
- EM RecipesDocument18 pagesEM RecipesSultan ShaikhNo ratings yet
- Furosemide 25491218 15Document26 pagesFurosemide 25491218 15ปรุฬห์ รุจนธำรงค์ (Parun Rutjanathamrong)No ratings yet
- Proses Pembuatan Hidrolisat Protein Ikan RucahDocument6 pagesProses Pembuatan Hidrolisat Protein Ikan RucahKhaerul FadlyNo ratings yet
- Initial Lab 5Document8 pagesInitial Lab 5Algenne AmiruddinNo ratings yet
- PHD IN ENGINEERING VIVA VOCE SLiDEDocument21 pagesPHD IN ENGINEERING VIVA VOCE SLiDEa.hawa.jasniNo ratings yet
- R3 - Produk Petrokimia Berbasis Gas - For Webinar 5 Jun 21Document18 pagesR3 - Produk Petrokimia Berbasis Gas - For Webinar 5 Jun 21MisbachulNo ratings yet
- 2019-04 Cosphatec Suggestions EN PDFDocument6 pages2019-04 Cosphatec Suggestions EN PDFZimzelena Kozmetika100% (1)
- Formula Disetujui "Lotion": Virgin Coconut OilDocument10 pagesFormula Disetujui "Lotion": Virgin Coconut Oilnyoman fitriNo ratings yet
- AB Indicators Indicators PDFDocument3 pagesAB Indicators Indicators PDFformoviejuneNo ratings yet
- Acid-Base Indicators PDFDocument3 pagesAcid-Base Indicators PDFAbu RaihanNo ratings yet
- Bouaouine2019 CactusDocument27 pagesBouaouine2019 CactusLaura CastiblancoNo ratings yet
- 10 - Drugs Containing LignansDocument10 pages10 - Drugs Containing LignansAmmy Joana Gallegos GarcíaNo ratings yet
- Physiol 93 B3Document1 pagePhysiol 93 B3DonkeyManNo ratings yet
- Pharm 02 A11Document4 pagesPharm 02 A11DonkeyManNo ratings yet
- CEACCP - Intrathecal Opioids in The Management of Acute Postoperative PainDocument5 pagesCEACCP - Intrathecal Opioids in The Management of Acute Postoperative PainDonkeyManNo ratings yet
- CEACCP - Latex AllergyDocument4 pagesCEACCP - Latex AllergyDonkeyManNo ratings yet
- CEACCP - KetamineDocument5 pagesCEACCP - KetamineDonkeyManNo ratings yet
- CEACCP - Illegal Substances in Anaesthetic and Intensive Care PracticesDocument5 pagesCEACCP - Illegal Substances in Anaesthetic and Intensive Care PracticesDonkeyManNo ratings yet
- Pharm 00 B14Document2 pagesPharm 00 B14DonkeyManNo ratings yet
- Pharm 00 A14Document2 pagesPharm 00 A14DonkeyManNo ratings yet
- Pharm 02 A10Document2 pagesPharm 02 A10DonkeyManNo ratings yet
- Pharm 00 B15Document2 pagesPharm 00 B15DonkeyManNo ratings yet
- Pharm 00 A15Document2 pagesPharm 00 A15DonkeyManNo ratings yet
- Pharm 00 A12Document1 pagePharm 00 A12DonkeyManNo ratings yet
- Pharm 00 B11Document1 pagePharm 00 B11DonkeyManNo ratings yet
- Compare and Contrast Neostigmine and The Organophosphate CompoundsDocument1 pageCompare and Contrast Neostigmine and The Organophosphate CompoundsDonkeyManNo ratings yet
- Pharm 00 A9Document2 pagesPharm 00 A9DonkeyManNo ratings yet
- Compare and Contrast The Pharmacology of Esmolol and PropanololDocument1 pageCompare and Contrast The Pharmacology of Esmolol and PropanololDonkeyManNo ratings yet
- Outline The Physiological Consequences of Hyperosmolar Diabetic KetoacidosisDocument2 pagesOutline The Physiological Consequences of Hyperosmolar Diabetic KetoacidosisDonkeyManNo ratings yet
- Compare and Contrast Atropine and Glycopyrulate, and Discuss The Clinical ImplicationsDocument2 pagesCompare and Contrast Atropine and Glycopyrulate, and Discuss The Clinical ImplicationsDonkeyManNo ratings yet
- Compare and Contrast The Pharamcology of Ephedrine and NoradrenalineDocument1 pageCompare and Contrast The Pharamcology of Ephedrine and NoradrenalineDonkeyManNo ratings yet
- Palliative Care HandbookDocument82 pagesPalliative Care HandbookDonkeyManNo ratings yet
- Define The Mechanisms of Action and Adverse Effects of Metoprolol, GTN, and Diltiazem When Used To Manage MIDocument2 pagesDefine The Mechanisms of Action and Adverse Effects of Metoprolol, GTN, and Diltiazem When Used To Manage MIDonkeyManNo ratings yet
- FS Antimicrobial Dosing Obesity AMS Updates Issue4 - Nov2018Document4 pagesFS Antimicrobial Dosing Obesity AMS Updates Issue4 - Nov2018DonkeyManNo ratings yet
- Cholinergic Agents: Cholinergic Receptors Types of Receptor Muscarinic Receptor Nicotinic ReceptorDocument4 pagesCholinergic Agents: Cholinergic Receptors Types of Receptor Muscarinic Receptor Nicotinic ReceptorDonkeyManNo ratings yet
- VOLATILEAGENTSDocument4 pagesVOLATILEAGENTSDonkeyManNo ratings yet
- Base Excess (Be) Measure of Metabolic Acid-Base Status: Dr. David LynessDocument1 pageBase Excess (Be) Measure of Metabolic Acid-Base Status: Dr. David LynessDonkeyManNo ratings yet
- Comparative Pharmacokinetics of Fentanyl and Alfentanil: Br. J. Anaesth. (1982), 54, 871Document7 pagesComparative Pharmacokinetics of Fentanyl and Alfentanil: Br. J. Anaesth. (1982), 54, 871DonkeyManNo ratings yet
- The Physiology of The GIT and The Liver QuestionsDocument44 pagesThe Physiology of The GIT and The Liver QuestionsDonkeyManNo ratings yet
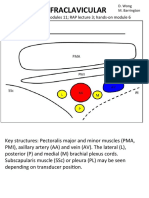
- Infraclavicular: Toolbox: Online Modules 11 RAP Lecture 3 Hands - On Module 6Document4 pagesInfraclavicular: Toolbox: Online Modules 11 RAP Lecture 3 Hands - On Module 6DonkeyManNo ratings yet
- USP-FCC Sugar Beet FiberDocument3 pagesUSP-FCC Sugar Beet FiberMAXNo ratings yet
- Madriz 2021Document5 pagesMadriz 2021pepeNo ratings yet
- Quality Evaluation and Shelf Life Assessment of Raw and Value Added Fish Product (Fish Cutlet) of Wallago Attu During Frozen Storage Conditions (-12)Document5 pagesQuality Evaluation and Shelf Life Assessment of Raw and Value Added Fish Product (Fish Cutlet) of Wallago Attu During Frozen Storage Conditions (-12)ajengNo ratings yet
- Acids and Bases Worksheet 1Document2 pagesAcids and Bases Worksheet 1lvstcoreNo ratings yet
- 2017 EJC H2 Chem Promos P1 Question PaperDocument11 pages2017 EJC H2 Chem Promos P1 Question PapernihaomaNo ratings yet
- Pulido RDocument119 pagesPulido RFelipe García VásquezNo ratings yet
- Ckp-Series DatasheetDocument10 pagesCkp-Series DatasheetSamylover Jean BaptisteNo ratings yet
- Softex CFCDocument2 pagesSoftex CFCkamalNo ratings yet
- Material For Table LegsDocument5 pagesMaterial For Table Legskutaiba AlmarzokiNo ratings yet
- TOS Dela PenaDocument8 pagesTOS Dela Penaarnel bulay-ogNo ratings yet
- Exp 2 Batch DistillationDocument11 pagesExp 2 Batch DistillationRansley TongNo ratings yet
- K01 - Group 1 - Production of Propylene Oxide - Mini Project Report - 12.6.22Document94 pagesK01 - Group 1 - Production of Propylene Oxide - Mini Project Report - 12.6.22Mars StudioNo ratings yet
- Class 10 Chemistry QuestionerDocument23 pagesClass 10 Chemistry QuestionerAnand HiremathNo ratings yet
- Review of Alumnia in Adsorption Karem-2021Document20 pagesReview of Alumnia in Adsorption Karem-2021Emilee Noven RamirezNo ratings yet
- The Truth About Urea: Ballang, Pancy Jane P. MTW 9:30AM-11:30AM BSN/1/4Document3 pagesThe Truth About Urea: Ballang, Pancy Jane P. MTW 9:30AM-11:30AM BSN/1/4PanJan BalNo ratings yet
- GBS Verrohrung 0114 ENDocument8 pagesGBS Verrohrung 0114 ENAlan TabourianNo ratings yet
- VALVES - 28 - Butteryfly - PVC and CPVCDocument17 pagesVALVES - 28 - Butteryfly - PVC and CPVCAdditya ChoudhharyNo ratings yet
- Trends in Corrosion Management - FinalDocument11 pagesTrends in Corrosion Management - FinalLuís PiresNo ratings yet
- Is.4941.1994Document10 pagesIs.4941.1994Omar BinshehabNo ratings yet
- Insufine VI 636Document3 pagesInsufine VI 636Karishma PrabhuNo ratings yet
- RSC Advances: ReviewDocument23 pagesRSC Advances: ReviewBurakTavşanlıNo ratings yet
- Chemical Reaction Engineering LAB MANUALDocument67 pagesChemical Reaction Engineering LAB MANUALkaviyas.21chemNo ratings yet