Professional Documents
Culture Documents
Chapter 6 Fitzpatrick's
Uploaded by
mylaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 6 Fitzpatrick's
Uploaded by
mylaCopyright:
Available Formats
2 Chapter 6 :: Skin Glands: Sebaceous, Eccrine,
and Apocrine Glands
:: Christos C. Zouboulis
INTRODUCTION ANATOMY OF THE
The human skin has several types of exocrine glands
(Latin, glandulae cutis), which release their biochemi-
SEBACEOUS GLANDS
cal products onto the skin surface. All skin glands
HISTOLOGY
Part 2
consist by a secretory compartment, the gland or coil
(tubulus), and an excretory part, the duct (ductus).
Human sebaceous glands are multilobular structures
Skin gland cells are of epithelial origin, but their
of epithelial origin that consist of acini connected to a
::
secretory compartments are located at different
common excretory duct, the sebaceous duct (ductus
depths in the dermis.
Structure and Function of Skin
seboglandularis) (Fig. 6-1). Sebaceous glands are com-
Three major types of skin glands are recognized
posed of sebocytes, which are lipid-producing uniquely
according to their product, the excretory function,
differentiated epithelial cells.1,2 On the other hand, the
and the location, where the excretory ducts release
sebaceous duct is lined by undifferentiated kerati-
their products (diseases of these glands are listed in
nocytes and is usually associated with a hair follicle
Table 6-1). Regarding their product, skin glands are
which is composed of stratified squamous epithelium.
classified into glands secreting sebum (sebaceous
The periphery of the sebaceous gland is a basal cell
glands) and sweat (sweat glands). Concerning their
layer composed of small, cuboidal, nucleated, highly
secretory function, skin glands are classified into
mitotic sebocytes.1,3 Cells progress toward the middle
holocrine glands, whose fully differentiated secretory
of the gland and accumulate lipid droplets (LDs) as
cells burst and release both the cytoplasmic content
they transform into terminally differentiated cells,
and the cell membranes into their ducts, and mero-
full of lipids.3 The latter lack all other cellular organ-
crine glands, which excrete their product via exo-
elles, burst, and die, excreting their entire contents to
cytosis from secretory cells. Regarding the location
the duct in a holocrine manner (Fig. 6-2). Surrounding
where their ducts release their product, the ducts of
the glands are connective tissue capsules composed of
sebaceous glands, in most cases, and apocrine sweat
collagen fibers that provide physical support.4
glands excrete their products into the hair follicle
canal, and the eccrine sweat glands excrete directly
onto the skin surface. Sebaceous glands are holocrine LOCATION
glands, and sweat glands (both eccrine and apocrine
ones) are merocrine glands. Sebaceous glands are associated with hair follicles all
over the body. A sebaceous gland associated with a
hair follicle is termed a pilosebaceous unit (see Fig. 6-1).
The glands may also be found in certain nonhairy
SEBACEOUS GLANDS sites, including the eyelids (Meibomian glands, tar-
sal glands), the nipples (Montgomery glands, areolar
glands), around the genitals (Tyson glands), and the
mucosa (lips, gums and inner cheeks, and genitals;
AT-A-GLANCE Fordyce spots).1 Fordyce spots open and release their
content directly to the epithelial surface. The latter are
■ Sebaceous glands are multilobular structures that visible to the unaided eye because of their large size
consist of acini connected to a common excretory (up to 2 to 3 mm) and the transparency of the oral epi-
duct and are usually associated with a hair follicle. thelium (Fig. 6-3). Only the palms and soles, which
■ Sebaceous glands vary considerably in size, even in have no hair follicles, are totally devoid of sebaceous
the same individual and in the same anatomic area. glands. In addition, the dorsal surfaces of the hand
■ The sebaceous glands excrete lipids by and foot have sparse sebaceous glands.5 Sebaceous
disintegration of entire cells, a process known as glands vary considerably in size, even within the
holocrine secretion. same individual and within the same anatomic area.
■ Human sebum, as it leaves the sebaceous gland, On the external body surface, most glands are only
contains squalene, cholesterol, cholesterol esters, a fraction of a millimeter in size. The largest glands
wax esters, and triglycerides. and greatest density of glands are located on the nose
(1600 glands/cm2) followed by the face and scalp (up
■ Sebaceous glands are regulated by several
to 400 to 900 glands/cm2).4 The hairs associated with
molecules, among them androgens and retinoids.
these large glands are often tiny, and the total structure
Kang_CH006_p0070-0088.indd 70 08/12/18 4:14 pm
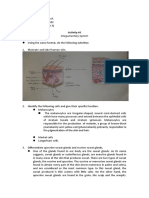
TABLE 6-1 Cross-section of a pilosebaceous unit
2
Diseases of the Major Skin Glands
Diseases of the Sebaceous Glands
Increased activity/volume Sebum
Acne vulgaris
Rosacea
(Hyper)seborrhea
Periorificial dermatitis SD
Hair follicle naevus
Congenital sebaceous gland hyperplasia SG
Senile sebaceous gland hyperplasia HF
Sebaceoma (sebaceous gland epithelioma)
Sebaceous carcinoma
Muir-Torre Syndrome
Chapter 6 :: Skin Glands: Sebaceous, Eccrine, and Apocrine Glands
Decreased activity/volume
Senile xerosis cutis
Psoriasis AP
Lichen planopilaris
Pseudopelade Brocq
Hidradenitis suppurativa
Linear morphea
Chlor- /dioxin-induced acne
Figure 6-1 Cross-section of a pilosebaceous unit: a mul-
Chemotherapy-induced diffuse alopecia
tiacinar sebaceous gkland associated with a hair follicle
Zouboulis syndrome
(HF). AP, arrector pili muscle (×20); SD, sebaceous duct,
Sebum, sebum and keratin. (Modified with permission
Diseases of the Eccrine Glands from: Zouboulis CC, Tsatsou F. Anatomy of the sebaceous
Increased activity gland. In: Zouboulis CC, Katsambas AD, Kligman AM, eds.
Hyperhidrosis (primary and secondary) Pathogenesis and Treatment of Acne and Rosacea. Berlin:
Eccrine carcinoma Springer; 2014:27-31. Copyright © 2014.)
Decreased activity
Hypohidrosis/Anhidrosis
Abnormal activity/Obstruction of the eccrine duct
Neutrophilic eccrine hidradenitis
13 to 16 weeks, the glands are clearly distinguishable,
Coma bullae arising in a cephalocaudal sequence from bulges (epi-
Erythema multiforme thelial placodes) of the hair follicles. The latter contain
Cystic fibrosis the epidermal stem cells that generate multiple cell lin-
Miliaria (crystallina, rubra, and profunda) eages, including epidermal and follicular keratinocytes,
Syringosquamous metaplasia) as well as sebaceous glands. As daughter cells migrate
Diseases of the Apocrine Glands from the bulge region, changes in the expression pat-
Abnormal activity terns of numerous transcription factors determine their
Bromhidrosis final cell lineage. Despite continuous differentiation of
Chromhidrosis its cells, the sebaceous gland can be regenerated by the
Fox-Fordyce disease (apocrine miliaria) reservoir of stem cells in the hair follicle bulge. How-
Hidradenitis suppurativa (initially considered as a disease of the ever, retroviral lineage marking has provided strong
apocrine glands; currently as a disease of the terminal hair follicles)
evidence that the sebaceous gland might arise and be
maintained independently of the hair follicle bulge.9
Wnt or wingless (Wnt) and Sonic hedgehog (Shh)
is more specifically termed sebaceous follicles, being a signaling pathways are intricately involved in embry-
pilosebaceous unit variant, the other two being the onic patterning and cell fate decisions. Cells destined to
terminal hair follicle and the vellus hair follicle. become sebocytes have increased Shh and Myc signaling
and decreased Wnt signaling (Fig. 6-4A).10,11 In human
SZ95 sebocyte and transgenic mouse models, whereas
EMBRYOGENESIS AND intact Wnt signaling promotes hair follicle differentia-
tion, inhibition of Wnt signaling by preventing the Lef1–
MORPHOGENESIS B-catenin interaction leads to sebocyte differentiation.11,12
Loss of function and gain of function in both models
The development of the sebaceous glands is closely demonstrated that blocking Shh signaling inhibited
related to the differentiation of hair follicles and normal sebocyte differentiation, and constitutively acti-
epidermis.6-8 At the 10th to 12th weeks of fetal life, a stra- vating Shh signaling increased the number and size of
tum intermedium becomes apparent, and at about the human sebocytes and mouse sebaceous glands in skin.
same time, developing hair germs are quite distinct. In Several important molecular aspects of sebaceous
the following weeks, the follicles extend downward into gland development have been identified, mostly
the dermis, and the rudiments of the sebaceous glands with the aid of genetically modified cell lines. The 71
appear on the posterior surfaces of the hair pegs. By earliest known signal necessary for sebaceous gland
Kang_CH006_p0070-0088.indd 71 08/12/18 4:14 pm
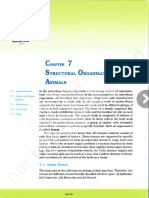
2 Hematoxylin and eosin-stained section of the
human sebaceous gland
Differentiation stages of human sebocytes
in tissue and in vitro
Early differentiated sebocytes
Basal sebocytes Connective tissue
Mature
Fully differentiated
Advanced
differentiated
Part 2
Early differentiated
::
Structure and Function of Skin
Undifferentiated
Fully differentiated and Advanced differentiated
(basal)
mature sebocytes sebocvtes
A B
Figure 6-2 A, Hematoxylin and eosin–stained section of the human sebaceous gland showing the different stages of
sebocyte differentiation. Cells progress toward the middle of the gland, lose their nuclei, and organelles, and accumulate
lipid droplets. B, Differentiation stages of human sebocytes in tissue (left)19 and in vitro (right)3 according to Tosti17 and
McEwan Jenkinson and coworkers.18 Undifferentiated sebocytes are small cells with a high nucleocytoplasmic ratio. Early
differentiated sebocytes are larger cells with a decreased nucleocyloplasmic ratio compared with the undifferentiated
sebocytes and a few lipid droplets arranged in the perinuclear area. Advanced differentiated sebocytes are cells with
further increases in size and decreases of the nucleocytoplasmic ratio. Multiple cytoplasmic lipid droplets are distributed
inside the cytoplasm. Fully differentiated sebocytes are cells with abundant, partially large, cytoplasmic lipid droplets.
Mature sebocytes are disorganized large cell with denatured nucelei; the lack of cytoplasmic lipids is caused by lysis of the
cell blood cell membrane.
development is SOX9, which is in fact essential for the Signaling pathways and transcription factors
specification of early hair follicle stem cells and there- in cell lineage determinations
fore for the morphogenesis of both structures (Fig. 6-5).9
Further studies indicate that later in embryonic devel- Stem cell
opment, a subpopulation of these stem cells expressing
PRDM1 (formerly known as BLIMP1) is established Tcf3
near the entrance of the sebaceous gland. PRDM1
(BLIMP-1) acts as a marker of terminal epithelial cell
differentiation.13,14 Loss of PRDM1 (BLIMP-1) results in Shh Wnt
increased gene expression of c-myc, an essential player Myc Lef1
in sebaceous gland homeostasis.15 Overexpression of
Wnt
Sebocyte Hair cell
Figure 6-4 Simplified signaling pathways and transcription
factors that are involved in cell lineage determinations.9-11
As daughter cells migrate from the bulge region, changes
in the expression patterns of numerous transcription fac-
tors determine their final cell lineage. Additional path-
ways and transcription factors play a significant role in
determining each cell lineage. Lef1, lymphoid enhancer
binding factor 1; Myc, myelocytomatosis oncogene; Shh,
72 Sonic hedgehog; Tcf3, transcription factor 3; Wnt, wingless
Figure 6-3 Fordyce spots at the upper lip mucosa. (wg)/int.
Kang_CH006_p0070-0088.indd 72 08/12/18 4:14 pm
Genes and their proteins/lipids that are involved in sebaceous differentiation and maturation
2
γ β/δ
Chapter 6 :: Skin Glands: Sebaceous, Eccrine, and Apocrine Glands
5
7
Figure 6-5 Genes and their proteins/lipids reported to be involved in sebaceous differentiation and maturation.9 PPAR,
peroxisome-proliferator-activated receptor.
c-myc in transgenic mice results in enlarged and more cells arranged in a single layer facing the basal lam-
numerous sebaceous gland at the expense of the hair ina, comparable to the epidermal basal layer; they
follicle lineage. Moreover, skin-specific deletion of represent the germinative cells of the gland, flattened
c-myc negatively affects sebaceous gland develop- or cuboidal in shape, showing round and densely
ment. In skin, c-myc and β-catenin exert opposing basophilic nuclei.20 These bear characteristics of stem
effects on sebocyte differentiation (see Fig. 6-4). Antag- cells because they give rise to a continual flux of pro-
onizing Wnt–β-catenin signaling constitutes an impor- liferating and differentiating cells. The basal cells of
tant prerequisite for normal sebaceous differentiation the peripheral zone form about 40% of the gland.
in postnatal skin tissue. Stem cells expressing LRIG1, Growing toward the center of the gland lobules, the
which has been suggested to be multipotent stem basal cells gradually differentiate into an early dif-
cells giving rise to epidermal lineages, can act under ferentiated cell type, an advanced differentiated cell
homeostatic conditions as sebocyte progenitor cells.16 type, a fully differentiated cell type, and the mature
Sebaceous gland cells at first contain glycogen. sebocyte.3,21 The maturation zone also represents
This lingers at the periphery of the gland but is about 40% of the sebaceous gland.
quickly lost at the center, where lipid drops are vis-
ible at 17 weeks.13,14 The future common excretory
duct, around which the acini of the sebaceous gland
attach, begins as a solid cord. The cells composing PHYSIOLOGY OF THE
the cord are filled with sebum, and eventually they
lose their integrity, rupture, and form a channel that SEBACEOUS GLAND
establishes the first pilosebaceous canal, the duct,
through which sebum flows into the follicular canal
and subsequently to the skin surface. New acini result
HOLOCRINE SECRETION
from buds on the peripheral sebaceous duct wall. The The sebaceous glands exude lipids by disintegration
cell organization of the neonatal sebaceous acini con- of entire cells, a process known as holocrine secretion.
sists of undifferentiated (basal), differentiating (early, Holocrine secretion by sebaceous gland cells does
advanced and fully differentiated), and mature seba- not occur mechanically via increased cell volume, as 73
ceous gland cells (see Fig. 6-2).3,17-19 Undifferentiated considered previously, but rather from a multistep,
Kang_CH006_p0070-0088.indd 73 08/12/18 4:14 pm
2 cell-specific lysosomal DNase2-mediated mode of
programmed cell death, which differs from apoptosis,
Human sebaceous gland lipids
necroptosis, and cornification.22
As sebaceous gland cells are displaced into the cen-
ter of the gland, they begin to produce lipids, which
accumulate in droplets. With approaching the seba- HO
ceous duct, they disintegrate and release their content. Squalene Cholesterol
Only neutral lipids reach the skin surface. Proteins,
nucleic acids, and the membrane phospholipids are
digested and are apparently recycled during the dis-
O
integration of the cells.2 Sebaceous gland secretion can
O
be enhanced with increased rates of induced terminal
sebocyte differentiation. Cholesterol ester
LIPID COMPOSITION OF SEBUM
Part 2
O
O
Sebum production is a continuous event. The exact
Wax ester
mechanisms underlying its regulation are not fully
::
defined. Complexity and uniqueness are the two terms
Structure and Function of Skin
O
that best characterize sebaceous lipids. ∆6 desatura- O
O
tion, wax ester synthesis, and squalene accumulation O O
are examples that manifest sebaceous lipid biology.22-24 O
Genetic knockout animal models of lipid synthesis
Triglyceride
demonstrate dramatic changes in skin physiology and
pathology, resulting from impairment of sebaceous
lipid pathways.25 Human sebum, as it leaves the seba- Figure 6-6 Human sebaceous gland lipids. The struc-
ceous gland, contains a mixture of nonpolar (neutral) tures of the cholesterol ester, wax ester, and triglyceride
lipids, mainly triglycerides, wax esters, squalene, and are representative of the many species that are present.
smaller amounts of cholesterol and cholesterol esters Two sebaceous-type unsaturated fatty acid moieties are
(Fig. 6-6). During passage of sebum through the hair shown: sapienic acid (16:1∆6) (in the wax ester structure)
canal, bacterial enzymes hydrolyze some of the tri- and sebaleic acid (18:2∆5,8) (in the triglyceride structure).
glycerides, so that the lipid mixture reaching the skin Anteiso branching is shown in the alcohol moiety of the
surface contains free fatty acids and small propor- wax ester, and iso branching is shown in the triglyceride.
tions of mono- and diglycerides, in addition to the
original components. Triglycerides, diglycerides, and
even-numbered carbon (internal branching). Exam-
free fatty acids form 40% to 60% of total skin surface
ples of these unusual unsaturated and branched-
lipids followed by wax esters (25% to 30%), squalene
chain moieties are included in the lipid structures
(12% to 15%), cholesterol esters (3% to 6%), and cho-
in Fig. 6-6.
lesterol (1.5% to 2.5%).26,27 The wax esters and squalene
distinguish sebum from the lipids of human internal
organs, which contain no wax esters and little squa- FUNCTION OF SEBUM
lene. However, human sebaceous glands appear to be
unable to transform squalene to sterols, such as cho- Sebum in humans was initially considered to solely
lesterol. The patterns of unsaturation of the fatty acids cause acne.28,29 Subsequently, it has been suggested
in the triglycerides, wax esters, and cholesterol esters that sebum reduces water loss from the skin’s surface
also distinguish human sebum from the lipids of other and functions to keep skin soft and smooth, although
organs. The “normal” mammalian pathway of desatu- evidence for these claims in humans is minimal; how-
ration involves inserting a double bond between the ever, as demonstrated in the sebaceous gland–deficient
9th and 10th carbons of stearic acid (18:0) to form (Asebia) mouse model, glycerol derived from triglyc-
oleic acid (18:1∆9). However, in human sebaceous eride hydrolysis in sebum is critical for maintaining
glands, the predominant pattern is the insertion of a stratum corneum hydration.30 Sebum has later been
∆6 double bond into palmitic acid (16:0). The resulting shown to have mild antibacterial action, protecting
sapienic acid (16:1∆6) (see Fig. 6-6) is the major fatty the skin from infection by bacteria and fungi because
acid of adult human sebum. Elongation of the chain it contains antiinflammatory lipids and immuno-
by two carbons and insertion of another double bond globulin A, which is secreted from most exocrine
gives sebaleic acid (18:2∆5,8), a fatty acid thought to be glands.31-33 Vitamin E delivery to the upper layers of
unique to human sebum.22-24 the skin protects the skin and its surface lipids from
Sebaceous fatty acids and alcohols are also distin- oxidation. Thus, sebum flow to the surface of the skin
guished by chain branching. Methyl branches can may provide the transit mechanism necessary for
occur on the penultimate carbon of a fatty acid chain vitamin E to function.34 The current concept is that
74 (iso branching), on the third from the last (ante- sebum is involved in the multimodal activities of the
penultimate) carbon (anteiso branching), or on any sebaceous glands (Table 6-2).
Kang_CH006_p0070-0088.indd 74 08/12/18 4:14 pm
TABLE 6-2
Propionibacterium acnes but also initiate cytokine pro-
duction and inflammation in the host organism.35,36 In
2
Sebaceous Gland Functions addition, free fatty acids in human sebum are bacte-
ricidal against gram-positive organisms as a result of
Embryology, Development, and Differentiation its ability to increase β-defensin 2 expression.31,36 Innate
■ Expression of terminal differentiation-triggering transcription
immune Toll-like receptors 2 and 4 (TLR2, TLR4) as
factors, including CCAAT and enhancer binding proteins and
well as CD1d and CD14 molecules are also expressed in
peroxisome-proliferator-activated receptors
sebaceous glands and immortalized human sebocytes.37
■ Partial responsibility for the three-dimensional organization of skin
surface lipids and the integrity of the skin barrier With the expression of innate immune receptors and
■ Influence on follicular differentiation antibacterial peptides, the sebaceous gland may play an
■ Highly complex acetylcholine receptor expression pattern important role in pathogen recognition and protection
■ Preservation of characteristics of stem-like cells despite their of the skin surface.38-41
terminal cell differentiation program
Synthetic Activity
■ Production of vernix caseosa
Chapter 6 :: Skin Glands: Sebaceous, Eccrine, and Apocrine Glands
■ Production of sebum
FACTORS REGULATING
■ Histamine-1 receptor expression and inhibition of squalene
synthesis by antihistamines
SEBACEOUS GLAND SIZE
Protection AND SEBUM PRODUCTION
■ Natural photoprotective activity against ultraviolet B irradiation
■ Thermoregulatory and repelling properties Sebocytes preserve characteristics of stem-like cells
■ Possible involvement in wound healing despite their programming for terminal differentia-
Transportation tion because they present a remarkable potential of
■ Delivery of antioxidants from and to the skin surface bipotential differentiation.42,43 The sebaceous gland
■ Sebum as vehicle of fragrance might be maintained by unipotent stem cells that are
Inflammation and Immunity replenished by multipotent stem cells in the hair fol-
■ Direct pro- and antiinflammatory properties licle bulge.13 However, it is an emerging view that there
■ Production of proinflammatory and of antiinflammatory lipids might be at least three distinct niches for skin stem
■ Toll-like receptor 2–induced upregulation of lipogenesis cells: the follicle bulge, the base of the sebaceous gland,
■ Lipid-induced innate antimicrobial activity and the basal layer of the epidermis.44
■ Presence of antimicrobial protective immunoglobulin A and
The average transit time of sebaceous gland cells
cytokine and chemokine mRNA in normal sebaceous glands
from formation to discharge, has been calculated
■ Synthesis of antibacterial peptides and proinflammatory cytokines
and chemokines in the presence of bacteria with some of the
as 7.4 days in the human gland, with 4 to 7 days in
peptides being bacteriotoxic undifferentiated and 14 to 25 in differentiated lipid-
■ Expression of ectopeptidases producing cells.1 Within any one glandular unit, the
■ Contribution to skin inflammation by promoting the differentiation acini vary in differentiation and maturity. The syn-
of Th17 lymphocytes thesis and discharge of the lipids contained in the
■ Response to lipid-mediated redox stress sebaceous cells require more than 1 week. The size of
■ Influence of macrophage polarization and activation via sebaceous glands increases with age. The mean size
sebaceous lipids rises from 0.2 mm2 ± 0.5 mm2 to 0.4 mm2 ± 2.1 mm2. The
Endocrine Properties sebaceous cells of prepubertal and hypogonadal boys
■ Regulation of the independent endocrine function of the skin and men are qualitatively similar to those of normal
■ Expression of all steroidogenic enzymes adults, even though the glands are smaller.45 In gen-
■ Regulation of local androgen synthesis eral, whereas the number of sebaceous glands remains
■ Substantial involvement in the hormonally induced skin aging
approximately the same throughout life, their size
process
tends to change with age.46 The turnover of the seba-
■ Modification of lipid synthesis by combined androgens and
peroxisome-proliferator-activated receptor ligands, estrogens and ceous glands in older adults is slowed down compared
the insulin-like growth factor 1–insulin-like growth factor 1 complex with young adults.
■ Expression of vitamin D receptor and vitamin D–metabolizing A variety of experimental models are used to study
enzymes the factors involved in sebaceous gland regulation,
■ Expression of retinoid-metabolizing cytochrome P450 enzymes including cell culture of isolated human sebaceous
■ Selective control of the action of hormones and xenobiotics on glands, primary sebocytes, immortalized sebocyte cell
the skin lines, and three-dimensional models, as well as mouse
■ Exhibition and affection by a regulatory neuropeptide program and hamster animal models.47-50 Results from these
investigations clearly indicate that sebaceous glands
are multifactional (see Table 6-2),51,52 regulated, among
INNATE IMMUNITY others, by ligands of sebaceous gland cell receptors
(Table 6-3), such as androgen and estrogen receptors,
Antimicrobial peptides, including cathelicidin, pso- peroxisome-proliferator-activated receptors (PPAR)
riasin, β-defensin 1, and β-defensin 2, are expressed and liver-X receptor (LXR), neuropeptide receptors,
within the sebaceous gland. Functional cathelicidin retinoid, and vitamin D receptors.53-56 The ligand– 75
peptides have direct antimicrobial activity against receptor complexes activate pathways involving
Kang_CH006_p0070-0088.indd 75 08/12/18 4:14 pm
2 TABLE 6-3
Hormone Receptors Expressed in Human Sebaceous Gland Cells
RECEPTORS NATURAL LIGANDS EFFECT ON CULTURED SEBOCYTES
Peptide Hormone and Neurotransmitter
Receptors
Serpentine (Seven-Transmembrane Domain)
Receptors
■ Corticotropin-releasing hormone (CRH) CRH, urocortin ↓ Proliferation, ↑ ∆5-4 3β-hydroxysteroid dehydrogenase
receptors 1 and 2 (CRH-R1 > CRH-R2) (CRH), ↑ lipid synthesis (CRH), ↑ IL-6 and IL-8 release
(CRH)
■ Melanocortin-1 and 5 receptors (MC-1R and α-Melanocyte-stimulating hormone ↓ IL-1–induced IL-8 synthesis (MC-5R), differentiation
MC-5R) (α-MSH) marker (MC-1R)
Part 2
■ µ-Opiate receptors (OPRs) β-Endorphin ↓ EGF-induced proliferation, ↑ lipid synthesis
■ VPAC receptors Vasoactive intestinal polypeptide (VIP), Neuropeptide Y stimulates IL-6 and IL-8 release
receptors for neuropeptide Y and cal-
::
citonin gene-related peptide (CGRP)
Structure and Function of Skin
■ Cannabinoid receptors CR1 and CR2 Cannabinoid
■ Histamine receptor 1 Histamine Regulation of squalene synthesis
Single-Transmembrane Domain Receptors
with Intrinsic Tyrosine Kinase Activity
■ Insulin-like growth factor (IGF) I receptor IGF-I, insulin ↑ Lipogenesis
Single-Transmembrane Domain Receptors
without Intrinsic Tyrosine Kinase Activity
■ Growth hormone (GH) receptor GH ↑ Differentiation, ↑ DHT effect on lipogenesis
Nuclear Receptors
Steroid Receptors
■ Androgen receptor Testosterone, 5α-dihydrotestosterone ↑ Proliferation (with PPAR ligands ↑ lipogenesis)
(DHT)
■ Progesterone receptor Progesterone ?
Thyroid Receptors
■ Estrogen receptors (ER-α- and -β) 17β-Estradiol ↑ Polar lipid production
■ Retinoic acid receptors (RAR-α and -γ) All-trans retinoic acid (atRA) ↓ Proliferation
■ Retinoid X receptors (RXR-α, > PXR-β, -γ) 9-cis RA Regulate lipogenesis (?)
■ Vitamin D receptor Vitamin D3 Regulates cell proliferation, cell cycle, lipid content, and
IL-6 and IL-8 secretion
■ Peroxisome proliferator-activated receptors Linoleic acid (RRARβ/∆), leukotrien-B4 ↑ Lipogenesis, ↑ prostaglandin E2 release, ↑ IL-6 release,
(PPARα, PPARγ > PPARβ) (LTB4) ↑ COX2 synthesis
■ Liver X receptors (LXRα and -β) 22(R)-Hydroxycholesterol ↓ Proliferation, ↑ lipogenesis, ↓ COX2 and inducible
NOS
COX, cyclooxygenase; DHT, 5α-dihydrotestosterone; EGF, epidermal growth factor; IGF, insulin-like growth factor; IL, interleukin; NO, nitric oxide synthase;
VPAC, vasoactive intestinal peptide receptor.
lipogenesis but also cell proliferation, differentiation, end-organ reduction product, 5α-dihydrotestosterone
hormone metabolism, and cytokine and chemokine (DHT), levels of testosterone do not parallel the pat-
release.57 terns of sebaceous gland activity. For example, testos-
terone levels are many fold higher in males than in
females, with no overlap between the sexes. However,
ANDROGENS the average rates of sebum secretion are only slightly
higher in males than in females, with considerable
Sebaceous glands require androgenic stimulation to overlap between the sexes. Also, sebum secretion starts
produce significant quantities of sebum. Individu- to increase in children during adrenarche, a develop-
als with a genetic deficiency of androgen receptors mental event that precedes puberty by about 2 years.
(complete androgen insensitivity) have no detectable The weak adrenal androgen, dehydroepiandros-
76 sebum secretion and do not develop acne.58 Although terone sulfate (DHEAS), is probably a significant regu-
the most powerful androgens are testosterone and its lator of sebaceous gland activity through its conversion
Kang_CH006_p0070-0088.indd 76 08/12/18 4:14 pm
to testosterone and DHT in the sebaceous gland.59
Levels of DHEAS are high in newborns, very low in
human sebaceous gland cells.68 In patients receiving
fibrates (PPAR-α ligands) for hyperlipidemia or thia-
2
2- to 4-year-old children, and start to rise when sebum zolidinediones (PPAR-γ ligands) for diabetes, sebum
secretion starts to increase. In adulthood, DHEAS secretion rates are increased.69
levels show considerable individual variation but are PPAR-γ–RXR-α and LXR–RXRα promoter inter-
only slightly higher in men than in women on the aver- actions are of crucial importance for the regulation
age. There is a decline in DHEAS levels in both sexes of key genes of lipid metabolism. Although vari-
starting in early adulthood and continuing throughout ous fatty acids, eicosanoids, and prostanoids acti-
life; this decline parallels the decline of sebum secre- vate PPARs, oxysterols and intermediate products
tion. DHEAS is present in the blood in high concentra- of the cholesterol biosynthetic pathway activate
tion. The enzymes required to convert DHEAS to more LXRs. PPAR-α agonists and PPAR-γ antagonists may
potent androgens are present in sebaceous glands.60 reduce sebaceous lipid synthesis and as such may be
These include 3β-hydroxysteroid dehydrogenase, useful in the treatment of acne. On the other hand,
17β-hydroxysteroid dehydrogenase, and 5α-reductase. whereas PPAR-γ agonists may be beneficial in aging
Chapter 6 :: Skin Glands: Sebaceous, Eccrine, and Apocrine Glands
Each of these enzymes exists in two or more isoforms skin, PPAR-δ agonists may be involved in sebaceous
that exhibit tissue-specific differences in their expres- tumorigenesis.
sion. The predominant isozymes in the sebaceous
gland include the type 1 3β-hydroxysteroid dehydro-
genase, the type 2 17β-hydroxysteroid dehydrogenase, LXR
and the type 1 5α-reductase.61,62
LXRs, which are members of the NHR family, play
a critical role in cholesterol homeostasis and lipid
metabolism.70 Treatment of SZ95 sebaceous gland
RETINOIDS cells with the LXR ligands TO901317 or 22(R)-
Isotretinoin (13-cis-retinoic acid, 13-cis-RA) is the most hydroxycholesterol enhanced accumulation of LDs in
potent pharmacologic inhibitor of sebum secretion. the cells, which could be explained through induction
Significant reductions in sebum production can be of the expression of the LXRα receptor and known LXR
observed as early as 2 weeks after use.63,64 Histologi- targets, such as fatty acid synthase and sterol regula-
cally, sebaceous glands are markedly reduced in size, tory element–binding protein-1 (SREBP-1).54,71
and individual sebocytes appear undifferentiated
lacking the characteristic cytoplasmic accumulation of
sebaceous lipids.3,65 FOXO1
Isotretinoin does not interact with any of the known
retinoid receptors. It may serve as a prodrug for the FoxO1 is expressed in most lipid-metabolizing cells,
synthesis of all-trans-retinoic acid, which interacts with including the prostate, liver, fat tissue, and skin.72
retinoid receptors expressed in sebaceous gland cells Human sebaceous gland cells also express FoxO1.
(retinoic acid receptors [RARs; isotypes α and γ] and ret- Acne and increased sebaceous lipogenesis are associ-
inoid X receptors [RXRs; isotypes α, β, γ]).66 However, it ated with a relative nuclear deficiency of FoxO1 caused
has greater sebosuppressive action than do all-trans- or by increased growth hormone–insulin–insulin-like
9-cis-retinoic acid.67 13-cis-RA exerts pluripotent effects growth factor 1 or fibroblast growth factor 2 signaling.
on human sebaceous gland cells and their lipogenesis.63
Inhibition of androgen synthesis, cell cycle arrest, and
apoptosis by 13-cis-RA may explain the reduction of
STRUCTURAL PROTEINS
sebaceous gland size after treatment. During sebogenesis, lipids are stored in LDs. LDs are
limited by a membrane containing phospholipids and
numerous proteins and enzymes. The most relevant
PEROXISOME-PROLIFERATOR- membrane proteins are the perilipin (PLIN) family,
ACTIVATED RECEPTORS which possesses structural and regulatory properties.
In particular, PLIN2, the major form expressed during
PPARs are members of the nuclear hormone receptor the differentiation process, regulates the gland size in
family and act as transcriptional regulators of a variety vivo and regulates sebaceous lipid accumulation.73
of genes, including those involved in lipid metabolism Experimental downmodulation of the PLIN2 expres-
in adipose tissue, liver, and skin. PPARs are similar to sion significantly modifies the composition of neutral
retinoid receptors in many ways. Each of these recep- lipids with a significant decrease in the unsaturated
tors forms heterodimers with retinoid X receptors fatty acid component caused by a marked decrease
to regulate the transcription of genes involved in a in the expression of specific lipogenic enzymes. On
variety of processes, including lipid metabolism and the other hand, PLIN3 has currently been shown to
cellular proliferation and differentiation. PPARα, δ, modulate specific lipogenic pathways in human seba-
and γ receptor subtypes have been detected in basal ceous gland cells.74 Another structural protein, angio-
sebaceous gland cells.54 PPARγ is also detected within poietin-like 4, is strongly induced during human
differentiated cells. Pharmacologic PPAR-γ modula- sebocyte differentiation and regulates sebaceous 77
tion regulates sebogenesis and inflammation in SZ95 lipogenesis.75
Kang_CH006_p0070-0088.indd 77 08/12/18 4:14 pm
2 CONCLUSION
are found over nearly the entire body surface and are
especially dense on the palms, soles, forehead, and
upper limbs.78 However, they are absent at the mar-
The regulation of sebaceous glands and human gins of the lips, the eardrums, and the nailbeds of
sebum production is complex. Advances are being fingers and toenails. Anlagen of eccrine sweat glands
made in this area, which may lead to alternative first appear in 3.5-month-old fetuses on the palms and
therapies for the reduction of sebum and improve- soles (see Chap. 4), then develop in the axillary skin
ments in acne. in the fifth fetal month, and finally develop over the
entire body by the sixth fetal month.78 The anlagen of
the eccrine sweat gland, which develops from the epi-
dermal ridge, is double layered and develops a lumen
SWEAT GLANDS between the layers between the fourth and eighth fetal
months. By the eighth fetal month, eccrine secretory
cells resemble those of an adult; by the ninth fetal
AT-A-GLANCE
Part 2
month, myoepithelial cells form around the secretory
coil and the excretory duct.
■ A human has 2 to 4 million sweat glands
::
(200 to 400/cm2 of skin surface).
■ ANATOMY AND FUNCTION OF THE
Structure and Function of Skin
Up to 10 L/day of sweat is produced by
acclimatized individuals. ECCRINE SWEAT GLANDS
■ In humans, sweat glands are generally classified
into apocrine and eccrine types. Two distinct segments, the secretory coil (tubulus) and
■ Hypothalamic temperature is the strongest
the duct, form the eccrine sweat gland. The secretory
stimulus for sweating.
coil secretes a sterile, dilute electrolyte solution with pri-
mary components of bicarbonate, potassium, sodium
■ Acetylcholine is the major stimulus of eccrine
chloride (NaCl), and other minor components such as
sweat glands secreted by sympathetic nerves.
glucose, pyruvate, lactate, cytokines, immunoglobulins,
■ Adrenergic stimulation controls apocrine gland antimicrobial peptides (eg, dermcidin,79 β-defensin,80
secretion. cathelicidines81). Relative to the plasma and extracellu-
■ Botulinum toxin inhibits sweating by preventing lar fluid, the concentration of Na+ ions is much lower in
acetylcholine release. sweat (∼40 mM versus ∼150 mM in plasma and extra-
■ Oxidative metabolism of glucose is a major source cellular fluid). The eccrine excretion has a high con-
of eccrine gland adenosine triphosphate. centration of Na+ ions. However, Na+ ions are partially
■ Ductal reabsorption conserves NaCl. reabsorbed via the epithelial sodium channels (ENaC)
that are located on the apical membrane of the eccrine
■ Bacteria are necessary for apocrine odor.
gland duct cells.82 This reuptake of Na+ ions reduces the
■ Odiferous precursors secretion is controlled by the loss of Na+ during the process of perspiration.
MRP8 encoded by ABCC11.
Secretory Coil: The secretory coil contains three
distinct cell types: (1) clear (secretory), (2) dark
(mucoid), and (3) myoepithelial.83 The clear and dark
Eccrine gland sweat allows the body to control its cells occur in approximately equal numbers but differ
internal temperature in response to thermal stress. in their distribution. Although the dark cells border
Apocrine gland function is more obscure but likely the apical (luminal) surfaces, the clear cells rest either
includes pheromone production. Although the eccrine directly on the basement membrane or on the on the
and apocrine secretory portions of sweat glands are myoepithelial cells. The clear cells directly access the
clearly morphologically distinctive, their ducts are lumen by forming intercellular canaliculi (Fig. 6-7).
histologically indistinguishable if the duct orifice can- Spindle-shaped contractile myoepithelial cells lie on
not be detected. Immunohistological distinction can be the basement membrane and abut the clear cells. An
performed by the stage-specific embryonic antigen-4 adult secretory coil is approximately 2- to 5-mm long
(SSEA-4), which is a marker of ductal cells of eccrine and approximately 30 to 50 µm in diameter. Heat accu-
but not of apocrine sweat glands.76 mulation results in larger sweat glands and ducts,
and their dimensions in turn correlate with enhanced
sweat output.84 Clear cells contain abundant mitochon-
ECCRINE SWEAT GLANDS dria and an autofluorescent body, called the lipofuscin
granule, in the cytoplasm. The clear cell plasma mem-
brane forms many villi. The clear cell secretes water
DEVELOPMENT OF THE ECCRINE and electrolytes. Dark cells have a smooth cell surface
SWEAT GLANDS and contain abundant dark cell granules.83 The func-
tion of dark cells is unknown. Myoepithelial cells con-
78 A human has approximately 2 to 4 million sweat tain actin filaments and are contractile,85,86 producing
glands (200 to 400/cm2 of skin surface).77 Sweat glands pulsatile sweat.
Kang_CH006_p0070-0088.indd 78 08/12/18 4:14 pm
Ultrastructure of the eccrine duct and secretory
coil and the localization of Na+, K+ -ATPase
2
Luminal cell Basal cell
Duct
(Lumen)
Chapter 6 :: Skin Glands: Sebaceous, Eccrine, and Apocrine Glands
Na+, K+-ATPase
Figure 6-7 Electron micrograph of the secretory coil of a Secretory
human eccrine sweat gland. B with arrow, basal lamina; coil
CC, clear cell; DC, dark cell; ICC, intercellular canaliculi; Lu,
lumen; MC, myoepithelial cell.
M
(Lumen)
C
Duct: The duct of the eccrine sweat gland consists
of an outer ring of peripheral or basal cells and an
IC
inner ring of luminal or cuticular cells. It seems that
the proximal (coiled) duct is functionally more active
Mc
than the distal straight portion in pumping Na+ for
C
ductal Na+ reabsorption because Na+, K+-adenosine
triphosphatase (ATPase) activity and the number D
of mitochondria are higher in the proximal portion
(Fig. 6-8).83,85,87,88 In contrast, the luminal ductal cells BM
have fewer mitochondria, much less Na+, K+-ATPase
activity, and a dense layer of tonofilaments near the
luminal membrane, which is often referred to as the
cuticular border. The cuticular border provides struc- Figure 6-8 The ultrastructure of the eccrine duct and
tural resilience to the ductal lumen, which may dilate secretory coil and the localization of Na+, K+-adenosine tri-
phosphatase (ATPase). The thick lines indicate the localiza-
whenever ductal flow of sweat is blocked. The entire
tion of Na+, K+-ATPase. BM, basement membrane; C, clear
structural organization of the duct is well designed cell; D, dark cells; IC, intercellular canaliculi; M, myoepithe-
for the most efficient Na+ absorptive function. The lial cell; Mc, mitochondria.
luminal membrane serves as the absorptive surface
by accommodating both Na+ and Cl− channels, and
the basal ductal cells serve in Na+ pumping by pro- of hypothalamic temperature associated with an
viding maximally expanded Na+ pump sites and increase in body temperature provides the strongest
efficient energy metabolism. The lumen and the duct stimulus for thermoregulatory sweating responses,
contain β-defensin, an antimicrobial, cysteine-rich, cutaneous temperature exerts a weaker influence on
low-molecular-weight peptide.80,81 In the epidermis, the rate of sweating.84,89 On a degree-to-degree basis,
the duct spirals tightly upon itself. an increase in internal temperature is about nine times
more efficient than an increase in mean skin tempera-
ture in stimulating the sweat center. The local tempera-
NEURAL CONTROL OF ture effect is speculated to be due to increased release
ECCRINE SWEATING of periglandular neurotransmitters.
The sweating in menopausal “hot flashes” rein-
The preoptic hypothalamic area plays an essential role forces the concept of a central hypothalamic mecha-
in regulating body temperature: whereas local heating nism for thermal sweating but also shows that the
of the preoptic hypothalamic tissue activates general- response of individuals to the same changes in core
ized sweating, vasodilatation, and rapid breathing, temperature can vary. Although hormonal factors
local cooling of the preoptic area causes generalized influence sweating during menopause, excessive 79
vasoconstriction and shivering. Whereas the elevation sweating does not correlate simply with hormonal
Kang_CH006_p0070-0088.indd 79 08/12/18 4:14 pm
2 levels. Instead, menopausal hot flashes seem to be
caused by a hypersensitive brain response (particu-
Botulinum toxin interferes with ACh release. Its
heavy chain binds the neurotoxin selectively to the
larly the hypothalamus but perhaps the insula, ante- cholinergic terminal, and the light chain acts within
rior cingulate, amygdala, and primary somatosensory the cells to prevent ACh release. Type A toxin cleaves
cortex as well). In asymptomatic menopausal women sensory nerve action potential-25, a 25-kDa synap-
and premenopausal women, the core temperature can tosomal-associated protein; the type B light chain
change up to 0.4°C (33°F) without eliciting a response. cleaves vesicle-associated membrane protein (also
In symptomatic postmenopausal women, changes as called synaptobrevin). Botulinum toxins are used for
small as 0.1°C (32°F) trigger peripheral vasodilation symptomatic relief of hyperhidrosis.93 A more detailed
and sweating. Why the brain is hypersensitive to small description can be found in Chaps. 81 and 216.
changes in core temperature is poorly understood, but
increased levels of brain norepinephrine appear to Denervation: In humans, the sweating response
influence the response to small changes in core tem- to intradermal injection of nicotine or ACh disappears
perature through their action on α2-adrenergic recep- within a few weeks after denervation of the postgangli-
onic fibers,93,94 and the sweating response to heat ceases
Part 2
tors in the brain; higher levels of the norepinephrine
metabolite 3-methoxy-4-hydroxyphenylglycol have immediately after resection of the nerves. In contrast,
also been found in symptomatic menopausal women after denervation of preganglionic fibers (caused by
compared with asymptomatic women. Decreased nor- spinal cord injuries or neuropathies), pharmacologic
::
epinephrine release is postulated as the mechanism by responsiveness of the sweat glands is maintained from
Structure and Function of Skin
which clonidine relieves hot flashes in symptomatic several months to 2 years, even though their thermally
women. Decreased core temperature may be the rea- induced sweating is no longer present.95
son that women with decreased body mass index tend
to have fewer symptoms even though their estrogen
levels probably are lower than those in women with
EMOTIONAL SWEATING
increased body mass index. Levels of estrogen, lutein- Sweating induced by emotional stress (emotional
izing hormone, and β-endorphins also were originally sweating) can occur over the whole skin surface in
thought to influence hot flashes, but later studies have some individuals, but it is usually confined to the
suggested no association.90 palms, soles, axillae, and forehead. Emotional sweat-
ing on the palms and soles ceases during sleep, but
Innervation: Efferent nerve fibers originating thermal sweating occurs even during sleep if the body
from the hypothalamic preoptic sweat center descend temperature rises. Because both types of sweating can
through the ipsilateral brainstem and medulla and be inhibited by atropine, emotional sweating is cholin-
synapse in the intermediolateral cell columns of the ergically medicated.
spinal cord without crossing (although sympathetic
vasomotor fibers may partially cross).91 The myelin-
ated axons rising from the intermediolateral horn of PHARMACOLOGY OF THE ECCRINE
the spinal cord (preganglionic fibers) pass out in the
anterior roots to reach (through white ramus commu-
SWEAT GLAND AND SWEATING RATE
nicans) the sympathetic chain and synapse. Unmyelin- Sweat glands respond to cholinergic agents, α- and
ated postganglionic sympathetic class C fibers arising β-adrenergic stimulants, and other periglandular neu-
from sympathetic ganglia join the major peripheral rotransmitters, such as vasoactive intestinal peptide
nerves and end around the sweat gland. The supply to and ATP. Periglandular ACh is the major stimulant of
the skin of the upper limb is commonly from T2 to T8. sweat secretion, and its periglandular concentration
The face and the eyelids are supplied by T1 to T4, so determines the sweat rate in humans.96 When dissoci-
that resection of T2 for the treatment of palmar hyperhi- ated clear cells are stimulated in vitro by cholinergic
drosis is likely to cause Horner syndrome. The trunk is agents, they lose K+ and Cl−, increase intracellular Ca2+,
supplied by T4 to T12 and the lower limbs by T10 to L2. and shrink, mimicking actions seen in vivo. Striking
Unlike the sensory innervation, a significant overlap individual differences exist in the degree of sweating
of innervation occurs in the sympathetic dermatome in response to a given thermal or physical stress. In
because a single preganglionic fiber can synapse with general, males perspire more profusely than females.97
several postganglionic fibers. The sweat rate in a given area of the skin is determined
The major neurotransmitter released from the peri- by the number of active glands and the average sweat
glandular nerve endings is acetylcholine (Ach), an rate per gland. The maximal sweat rate per gland var-
exception to the general rule of sympathetic inner- ies from 2 to 20 nL/min2. Sweat rate increases during
vation, in which noradrenaline is the peripheral acclimatization, but the morphologic and pharmaco-
neurotransmitter.92 In addition to ACh, adenosine tri- logic bases of the individual and regional differences
phosphate (ATP), catecholamine, vasoactive intestinal in sweating rate during acclimatization are still poorly
peptide, atrial natriuretic peptide, calcitonin gene- understood (Fig. 6-9). In thermally induced sweating,
related peptide, and galanin have been localized in the the sweat rate can be mathematically related to the
periglandular nerves. The significance of these pep- body and skin temperatures in a given subject only
80 tides or neurotransmitters in relation to sweat gland in the low sweat rate range. Cholinergic stimulation
function is not fully understood. yields a 5 to 10 times higher sweating rate than does
Kang_CH006_p0070-0088.indd 80 08/12/18 4:14 pm
ENERGY METABOLISM 2
Sweat secretion is mediated by the energy (ie, ATP)-
dependent active transport of ions, so a continuous
supply of metabolic energy is mandatory for sustained
sweat secretion. Endogenous glycogen stored in the
clear cells can sustain sweat secretion for less than
10 minutes; thus, the sweat gland must depend almost
exclusively on exogenous substrates for its energy
metabolism. Mannose, lactate, and pyruvate are used
nearly as readily as glucose; other hexoses, fatty acids,
ketone bodies, intermediates of the tricarboxylic acid
cycle, and amino acids are either very poorly used or
not used as substrates. The physiologic significance
Chapter 6 :: Skin Glands: Sebaceous, Eccrine, and Apocrine Glands
of lactate or pyruvate utilization by the sweat gland
Figure 6-9 Individual variation in the size of the sweat is not yet clear. However, because the plasma level of
gland in four male adults, aged 22 to 28 years. Sweat glucose (5.5 mM) is much higher than that of lactate
glands were isolated from skin biopsy specimens obtained (1 to 2 mM) or pyruvate (<1 mM), glucose may play a
from the upper back behind the axilla. Whereas subject 1 major role in sweat secretion. Oxidative metabolism of
is a sedentary man who does not exercise regularly, sub-
glucose is favored as the major route of ATP formation
ject 4 is a well-acclimatized athletic individual.
for secretory activity.100
β-adrenergic stimulation. α-Adrenergic stimulation
(by phenylephrine) is no more potent than isoproter-
COMPOSITION OF HUMAN
enol (ISO) (a β-adrenergic agonist) in humans in vivo.98 ECCRINE SWEAT
Whereas cholinergic sweating begins immediately on
intradermal injection, β-adrenergic sweating requires
Inorganic Ions: Sweat is formed in two steps:
(1) secretion of a primary fluid containing nearly iso-
a latent period of from 1 to 2 minutes, which suggests
tonic NaCl concentrations by the secretory coil and
that the intracellular mechanism of sweat induction
(2) reabsorption of NaCl from the primary fluid by
may be different for methacholine and for ISO. Because
the duct. Although a number of factors affect ductal
the sweat rate in response to adrenergic agents is rather
NaCl absorption, the sweat rate (and thus the tran-
low, it may be reasonable to surmise that adrenergic
sit time of sweat) has the most important influence
stimulation in periglandular nerves may be involved
on final NaCl concentration. Sweat NaCl concentra-
in the regulation of sweat gland function but not in the
tion increases with increasing sweat rate to plateau at
induction of sweat secretion. One consequence of dual
around 100 mM (Fig. 6-10). Potassium (K+) concentra-
cholinergic and adrenergic innervation is to maximize
tion in sweat is relatively constant. It ranges from 5 to
tissue accumulation of cyclic adenosine monophos-
10 mM, which is slightly higher than plasma K+ con-
phate (cAMP), which may be instrumental in stimulat-
centration. HCO3− concentration in the primary sweat
ing the synthesis of sweat and glandular hypertrophy
fluid is approximately 10 mM, but that of final sweat
of the sweat gland. The possibility that periglandular
is less than 1 mM, which indicates that HCO3− is reab-
catecholamine is directly involved in emotional sweat-
sorbed by the duct, presumably accompanied by ductal
ing or sweating associated with pheochromocytoma99
acidification.101 Sweat NaCl concentration is increased
may be ruled out because these sweating responses
in individuals with cystic fibrosis.102 Aquagenic wrin-
can be blocked by anticholinergic agents.
kling of the palms (whitened, wrinkling, and papil-
lation of the palms after brief water exposure) is seen
more frequently in carriers and patients with cystic
PHARMACOLOGY AND FUNCTION fibrosis (see Chap. 81).
OF ECCRINE MYOEPITHELIUM Lactate: The concentration of lactate in sweat usu-
ally depends on the sweat rate. At low sweat rates,
The periodicity of sweat secretion in vivo is caused by lactate concentration is as high as 30 to 40 mM, but it
the periodicity of central nerve impulse discharges, rapidly drops to a plateau at around 10 to 15 mM as
which occur synchronously with vasomotor tonus the sweat rate increases. Whereas acclimatization is
waves. Myoepithelial contraction occurs with choliner- known to lower sweat lactate concentrations, arterial
gic stimulation, but neither α- nor β-adrenergic agents occlusion rapidly raises sweat NaCl and lactate con-
induce tubular contraction.100 Although the myoepi- centrations and reduces the sweat rate.100 Sweat lactate
thelium may contribute to sweat production via pul- is probably produced by glycolysis of glucose by the
satile contractions, it also seems to provide structural secretory cells.103
support for the secretory epithelium, especially under
conditions in which stagnation of sweat flow (caused Urea: Urea in sweat is derived mostly from serum
by ductal blockade) results in an increase in luminal urea.104 Sweat urea content is usually expressed as a
81
hydrostatic pressure.86 sweat–plasma ratio (S/P urea). S/P urea is high (2 to 4)
Kang_CH006_p0070-0088.indd 81 08/12/18 4:14 pm
2 Sweat ingredients vs. sweat rates
sweat.79 Other organic compounds reported to be pres-
ent in sweat include histamine,109 prostaglandin,110 and
vitamin K–like substances.111 Sweat also contains traces
Hydration
of pyruvate and glucose. Sweat glucose increases con-
100
currently with a rise in plasma glucose level. Some
orally ingested drugs, including griseofulvin,112
Na+ and Cl–
in CF ketoconazole,113 amphetamines,114 and various chemo-
80
therapeutic agents,115 are secreted in sweat.
Na+
60
Cl–
Lactate MECHANISMS OF SWEAT
Concentration (mM)
40 K+ SECRETION
Urea
20 Ammonia Several distinct sequential processes lead to eccrine
Part 2
gland sweat production116: (1) stimulation of the eccrine
0 sweat gland by ACh via increased intracellular Ca2+;
(2) Ca2+-stimulated loss of cellular K+, Cl−, and H2O,
Pyruvate which leads to eccrine gland cell shrinkage; and (3)
::
1.0
Total Ca2+ volume-activated transcellular plus paracellular fluxes
Structure and Function of Skin
Free Ca2+
0.3 of Na+, Cl−, and H2O, which leads to net flux of largely
Glucose
0.2 isotonic NaCl solution into the glandular lumen. These
processes are illustrated in Fig. 6-11.
0.1 Sweating initially is stimulated when ACh is
0 released from periglandular cholinergic nerve endings
0 1 2 3 4 in response to thermal or emotional stimuli. ACh binds
Sweat rate (mL/min/cm2) to cholinergic receptors on the clear cell plasma mem-
brane, stimulating intracellular Ca2+ release and influx,
Figure 6-10 Relationship between the concentration of and increasing cytosolic Ca2+ concentrations. Increased
sweat ingredients and the sweat rate in thermally induced intracellular Ca2+, in turn, opens Ca2+-sensitive Cl− and
human sweat in normal individuals and in persons with K+ channels in the clear cell basolateral membrane,
cystic fibrosis (CF). which allows Cl− and K+ to escape. Because H2O fol-
lows K+ and Cl−, to maintain cell iso-osmolarity, the cell
shrinks.116,117
at a low sweat rate range but approaches a plateau at This decrease in cell volume sets off a second cascade
1.2 to 1.5 as the sweat rate increases. of cell signaling events. First, decreased cell volume
Ammonia and Amino Acids: The ammonia stimulates the NKCC1118 class of Na/K/2Cl cotrans-
concentration in sweat is 0.5 to 8 mM,105 which is 20 to porters, which carry Na+, K+, and 2Cl− into the cell in
50 times higher than the plasma ammonia level. The an electrically neutral fashion (ie, two cations and two
concentration of sweat ammonia is inversely related anions cancel out net charges). The resulting increase in
to the sweat rate and sweat pH. Free amino acids are cytosolic Na+ activates the Na+, K+-ATPase, located in the
present in human sweat,106 although it is not clear what basolateral membrane, which recycles Na+ and K+ across
proportion of measured amino acids derive from epi- the basolateral membrane. The net movement of the
dermal contamination. negatively charged Cl− ion across the apical membrane
into the lumen in turn drives the positively charged Na+
Proteins Including Proteases: The concen- ion into the lumen as well, along a paracellular pathway.
tration of sweat protein in the least contaminated, Therefore, the final product of glandular secretion is the
thermally induced sweat is approximately 20 mg/dL, net movement of Na+, Cl−, and H2O into the glandular
with the major portion being low-molecular-weight lumen to form the isotonic NaCl precursor of sweat.
proteins (ie, molecular weight <10,000). Because sweat ACh-induced sweating, which constitutes the bulk
samples collected by simple scraping (and even those of sweat production, appears to be mediated by intra-
collected with a plastic bag) can be massively contami- cellular Ca2+, as detailed earlier. In contrast, adrenergic-
nated with plasma or epidermal proteins, previous induced sweating appears to be mediated by increased
reports on the presence of α- and γ-globulins, transfer- intracellular cAMP.119
rin, ceruloplasmin, orosomucoid, albumin,106,107 and
immunoglobulin E must be carefully reexamined. The
sweat samples collected over an oil barrier placed on MECHANISM OF DUCTAL
the skin (the least-contaminated sweat) contain no or REABSORPTION
trace of γ-globulin and a very small amount of albu-
min. Yokozeki and coworkers108 also reported the pres- Because the production of large sweat volumes could
ence of cysteine proteinases and their endogenous lead to dangerous losses of NaCl, the sweat duct has
82 inhibitors in sweat and the sweat gland. Dermcidin evolved to reabsorb NaCl, which minimizes electrolyte
is an antimicrobial peptide produced and secreted in loss, even at high sweat volumes (Fig. 6-12).
Kang_CH006_p0070-0088.indd 82 08/12/18 4:14 pm
Modified Na/K/Cl cotransport model
surface.121 Unlike in the lung, CFTR mutations do not
lead to increased ENaC-mediated Na+ influx, which
2
ACh suggests that the CFTR–ENaC interactions seen in
other tissues differ from that in the eccrine duct. Sweat
CI– acidification appears to be mediated via the enzyme
Ca2+ carbonic anhydrase, the HCO3−/Cl and Na+/H+
exchangers, and the V-type H+ ATPase. The intracellu-
lar enzyme carbonic anhydrase catalyzes HCO3− and
K+ H+ production. Whereas intracellular HCO3− is cleared
via the HCO3−/Cl antiporter, H+ is pumped into the
H2O luminal sweat by the V-type H+ ATPase.122 The Na+/H+
B
antiporter NHE1 (Na+/H+ exchanger isoform 1),123,124
L
found in the basolateral membrane, is important in
Cell shrinkage intracellular pH regulation.
Na+
Chapter 6 :: Skin Glands: Sebaceous, Eccrine, and Apocrine Glands
The transfer of sweat to the skin surface without
K+ leakage is important for the homeostatic regulation of
2CI–
skin and is impaired in atopic dermatitis; lesional skin
CI– presents a decreased claudin-3 expression in sweat
glands, which is accompanied by sweat leakage.122
Several drugs are known to modify ductal NaCl reab-
Na+
sorption. When aldosterone is injected systemically
K+ or locally, the Na/K ratio in sweat begins to decrease
within 6 hours, reaching a nadir at 24 hours and
returning to the preinjection level in 48 to 72 hours.121
Na+ Na+ deprivation stimulates both renin and aldoste-
rone secretion, but high thermal stress per se (a single
1-hour exposure of humans to a temperature of 40°C
Figure 6-11 Modified Na/K/2Cl cotransport model for the
[104°F]) is a potent stimulator of renin and aldosterone
ionic mechanism of cholinergic eccrine sweat secretion.
Periglandular neurotransmitters, such as acetylcholine secretion in either the presence or absence of sodium
(ACh), bind to receptors on the basolateral membrane, deprivation. In an in vitro sweat gland preparation,
which leads to increased intracellular Ca2+; this in turn acti- neither acetazolamide (a carbonic anhydrase inhibitor)
vates K+ and Cl− channels, mediating K+, Cl–, and H2O efflux nor antidiuretic hormone changed ductal or secretory
from the cell. The resulting cell shrinkage activates the function. However, more potent carbonic anhydrase
basolateral Na+/K+/2Cl antiporter, which leads to Na+, K+, inhibitors, such as topiramate,125 have been reported to
and Cl− influx. The Na+ and K+ fluxes are recycled across the induce oligohidrosis.
basolateral membrane by the Na+, K+-adenosine triphos-
phatase. In contrast, Cl− fluxes flow unopposed into the
lumen, causing an electrical gradient that drives Na+ exit
from the tissue into the lumen via a paracellular pathway. APOCRINE SWEAT GLANDS
Net fluxes: H2O, Cl–, and Na+ (isotonic) flow into the lumen.
pH of the secreted fluid is neutral. Paracellular Na+ fluxes
Apocrine sweat glands are found in humans, largely
across the cell junction are indicated with an arrow at the
bottom of the figure. B, basolateral membrane; L, luminal confined to the regions of the axillae, the perineum,
or apical membrane. and the areolae of the breast.126 Differentiated apo-
crine sweat glands are present at the external audi-
tory canal (ceruminous glands). Apocrine sweat
Ductal Na+ reabsorption is accomplished through glands do not become functional until just before
the coordinated activities of intracellular enzymes puberty; thus, it is assumed that their develop-
and plasma membrane ion channels, pumps, and ment is associated with the hormonal changes at
exchangers. These mechanisms not only reabsorb puberty, although the exact hormones have not been
electrolytes but also acidify the sweat, which results in identified.
a final sweat product that is hypotonic and acidic. Na+
reenters the duct cells through the apical membrane
via amiloride-sensitive120 epithelial Na+ channels
ANATOMY
(ENaC)5 and is transported across the basolateral mem- Apocrine glands are coiled and localized in the sub-
brane by ouabain-sensitive88 Na+, K+-ATPase pumps. cutaneous fat near the dermis. The gland consists of a
Cl− transport appears to be both transcellular and single layer of cuboidal or columnar cells. These secre-
paracellular, with the cystic fibrosis transmembrane tory cells rest on a layer of myoepithelial cells.127 The
regulator (CFTR) Cl− channels playing an important duct is composed of a double layer of cuboidal cells
role in transcellular fluxes.118 In cystic fibrosis, CFTR and empties into hair follicle infundibulum. Sweat and
Cl− channels are mutated, and eccrine duct Cl− reab- sebum are mixed in the hair follicle and arrive mixed
sorption is defective but not completely abolished.27 at the epidermal surface. The apocrine sweat is cloudy, 83
Na+ is increased in the duct and the sweat at the skin viscous, initially odorless, and at a pH of 6 to 7.5.
Kang_CH006_p0070-0088.indd 83 08/12/18 4:14 pm
2 Ion reabsorption in the sweat duct
L B
CI–
CA Na+
K+
H2O + CO2 H++HCO3–
H+ CI–
H+V–ATPase
HCO3–
CI+
(CFTR)
Na+ H+
(NHE1)
(ENaC)
Na+
Part 2
CI–
Figure 6-12 Illustration of ion reabsorption in the sweat duct. Na+ enters the apical (luminal) membrane through epithelial
::
Na+ channels (ENaC) and is transported across the basolateral membrane by Na+, K+-adenosine triphosphatase (ATPase).
Structure and Function of Skin
Cl− enters the cell through the cystic fibrosis transmembrane regulator Cl− channel (CFTR) and is transported across the
lumen via a paracellular pathway. H+ generated by the enzyme carbonic anhydrase (CA) is pumped into the lumen by
a V-type H+ ATPase (H+ V-ATPase). Intracellular pH homeostasis is maintained by parallel HCO3–/H+ and Na+/H+ (NHE1)
exchangers. The activity of these enzymes, transporters, and channels results in H+ secretion and Na+ and Cl− reabsorption,
which produces a final sweat that is hypotonic and acidic. Paracellular Cl− fluxes across the cell junction are indicated with
an arrow at the bottom of the figure. B, basolateral membrane; L, luminal or apical membrane.
The sweat of apocrine sweat glands only attains its COMPOSITION OF SECRETION
characteristic odor upon being degraded by bacteria,
which releases volatile odor molecules. More bacte- When it is first secreted, the apocrine sweat of humans
ria (especially corynebacteria) leads to stronger odor. is milky, viscid, and without odor. Apocrine sweat
The presence of axillary hair also makes the odor even contains three types of precursors: fatty acids, sulfanyl
more pungent because secretions, debris, keratin, and alkanols, and odiferous steroids, which are converted
bacteria accumulate on the hair. by bacteria on axillary skin, particularly corynebacte-
Like the eccrine gland, the myoepithelium fulfills rium striatum, into odiferous substances. Secretion of
dual functions in both providing structural support amino acid and steroid precursors is controlled by an
and pumping out preformed sweat. ATP-dependent efflux pump multidrug resistance pro-
β-Adrenergic receptors and purinergic receptors tein 8 (MRP8), encoded by the gene ABCC11, which is
have been identified on apocrine glands.94 However, expressed in apocrine sweat glands. Axillary odor is
nerve fibers and muscarinic receptors have not been significantly reduced in Asian populations that carry
identified, suggesting that any cholinergic stimulation a single nucleotide polymorphism in this gene, which
acts humorally.128 also affects earwax characteristics.130
FUNCTIONS MODE OF SECRETION
A number of functions have been attributed to the Despite previous reports for apocrine (decapitation),
apocrine glands, including roles as odoriferous sexual holocrine, and merocrine types of secretion in apocrine
attractants, territorial markers, and warning signals. glands, current data indicate that the secretion of apo-
These glands play a role in increasing frictional resis- crine glands is merocrine. Cannulation of the duct of
tance and tactile sensibility as well as in increasing the human apocrine sweat gland has shown that secre-
evaporative heat loss in some species. The production tion is pulsatile, and it is assumed that contractions of
of pheromones by the apocrine glands of many species the myoepithelial cells surrounding the secretory cells
is well established.129 are responsible for these pulsations.131
Because the apocrine glands of humans do not begin
to function until puberty and are odor producing, it
is attractive to speculate that they have some sexual
CONTROL OF SECRETION
function, which may now be vestigial. There are high The apocrine sweat glands of humans respond to emo-
levels of 15-lipoxygenase-2 in the secretory cells of tive stimuli only after puberty. They can be stimulated
the apocrine gland. Its product, 15-hydroxyeicosatet- by either epinephrine or norepinephrine given locally
raenoic, a ligand for the nuclear receptor PPARγ, may or systemically. Studies have shown that the apocrine
84 function as a signaling molecule and in secretion or glands are controlled mainly by adrenergic agonists,132
differentiation.128 although some cholinergic control also has been
Kang_CH006_p0070-0088.indd 84 08/12/18 4:14 pm
reported.128,133 This is in contrast to the eccrine glands,
which are under cholinergic control.
13. Lo Celso C, Berta MA, Braun KM, et al. Characteriza-
tion of bipotent epidermal progenitors derived from
2
Although an intact nerve supply is a functional human sebaceous gland: contrasting roles of c-myc
requirement of apocrine sweating, the demonstration and β-catenin. Stem Cells. 2008;26:1241-1252.
of nerve endings or varicosities in close proximity to 14. Magnúsdóttir E, Kalachikov S, Mizukoshi K, et al.
Epidermal terminal differentiation depends on B
the glands has been difficult.128,133 Local capillary circu-
lymphocyte-induced maturation protein-1. Proc Natl
lation likely assists in conveying transmitter substance Acad Sci U S A. 2007;104:14988–14993.
to the sweat gland cells, a form of neurohumoral 15. Horsley V, Elder HY, Montgomery I, et al. Blimp1
transmission. defines a progenitor population that governs cel-
As would be expected, drugs that affect adrenergic lular input to the sebaceous gland. Cell. 2006;126:
systems also have an effect on apocrine sweat glands. 597-609.
Adrenergic neuron-blocking agents inhibit sweating, 16. Niemann C, Horsley V. Development and homeosta-
as do drugs that deplete the stores of transmitter sub- sis of the sebaceous gland. Semin Cell Dev Biol. 2012;
stance in adrenergic neurons. Drugs that block spe- 23:928-936.
17. Tosti A. A comparison of the histodynamics of seba-
Chapter 6 :: Skin Glands: Sebaceous, Eccrine, and Apocrine Glands
cific adrenergic receptors also inhibit sweating, but
ceous glands and epidermis in man: a microanatomic
the types of receptors that must be blocked differ in
and morphometric study. J Invest Dermatol. 1974;
various species. The type of receptor that mediates the 62:147-152.
response of the apocrine glands of humans has not 18. Jenkinson DM, Elder HY, Montgomery I, et al. Com-
been elucidated. parative studies of the ultrastructure of the seba-
ceous gland. Tissue Cell. 1985;17:683-698.
19. Kurokawa I, Mayer-da-Silva A, Gollnick H, et al. Mono-
clonal antibody labeling for cytokeratins and filag-
REFERENCES grin in the human pilosebaceous unit of normal,
seborrhoeic and acne skin. J Invest Dermatol. 1988;
1. Zouboulis CC, Fimmel S, Ortmann J, et al. Sebaceous 91:566-571.
glands. In: Hoath SB, Maibach HI, eds. Neonatal 20. Zouboulis CC, Tsatsou F. Anatomy of the sebaceous
Skin—Structure and Function, 2nd ed. New York: gland. In: Zouboulis CC, Katsambas AD, Kligman AM,
Marcel Dekker; 2003:59-88. eds. Pathogenesis and Treatment of Acne and Rosacea.
2. Pappas A. Sebum and sebaceous lipids. In: Zouboulis Berlin: Springer; 2014:27-31.
CC, Katsambas AD, Kligman AM, eds. Pathogenesis 21. Xia L, Zouboulis C, Detmar M, et al. Isolation of human
and Treatment of Acne and Rosacea. Berlin: Springer; sebaceous glands and cultivation of sebaceous gland-
2014:33-41. derived cells as an in vitro model. J Invest Dermatol. 1989;
3. Zouboulis CC, Krieter A, Gollnick H, et al. Progressive 93:315-321.
differentiation of human sebocytes in vitro is charac- 22. Fischer H, Fumicz J, Rossiter H, et al. Holocrine secre-
terized by increased cell size and altered antigenic tion of sebum is a unique DNase2-dependent mode
expression and is regulated by culture duration and of programmed cell death. J Invest Dermatol. 2017;
retinoids. Exp Dermatol. 1994;3:151-160. 137:587-594.
4. Downie MMT, Guy R, Kealey T. Advances in sebaceous 23. Nicolaides N. Skin lipids: their biochemical unique-
gland research: potential new approaches to acne ness. Science. 1974;186:19-26.
management. Int J Cosmet Sci. 2004;26:291-311. 24. Picardo M, Ottaviani M, Camera E, et al. Sebaceous
5. Benfenati A, Brillanti F. Sulla distribuzione delle ghi- gland lipids. Dermatoendocrinol. 2009;1:68-71.
andole sebacee nella cute del corpo umino. Arch Ital 25. Georgel P, Crozat K, Lauth X, et al. A TLR2-responsive
Dermatol. 1939;15:33-42. lipid effector pathway protects mammals against
6. Montagna W. An introduction to sebaceous glands. Gram-positive bacterial skin infections. Infect Immun.
J Invest Dermatol. 1974;62:120-123. 2005;73:4512-4521.
7. Thody AJ, Shuster S. Control and function of 26. Camera E, Ludovici M, Galante M, et al. Comprehensive
sebaceous glands. Physiol Rev. 1989;69:383-416. analysis of the major lipid classes in sebum by rapid
8. Deplewski D, Rosenfield RL. Role of hormones in pilo- resolution high-performance liquid chromatography
sebaceous unit development. Endocrine Rev. 2000; and electrospray mass spectrometry. J Lipid Res. 2010;
21:363-392. 51:3377-3388.
9. Zouboulis CC, Nikolakis G, Dessinioti C. Molecular 27. Nikkari T. Comparative chemistry of sebum. J Invest
aspects of sebaceous differentiation. In: Zouboulis Dermatol. 1974;62:257-267.
CC, Katsambas AD, Kligman AM, eds. Pathogenesis 28. Kligman AM. The uses of sebum? In. Montagna W,
and Treatment of Acne and Rosacea. Berlin: Springer; Ellis RA, Silver AF, eds. Advances in Biology of Skin. Vol
2014:19-26. IV. The Sebaceous Glands. Oxford: Pergamon Press;
10. Merrill B, Gat U, DasGupta R, et al. Tcf3 and Lef1 regu- 1963:110-112.
late lineage differentiation of multipotent stem cells 29. Cunliffe WJ, Shuster S. Pathogenesis of acne. Lancet.
in skin. Genes Dev. 2001;15:1688-1705. 1969;1(7597):685-687.
11. Niemann C, Unden AB, Lyle S, et al. Indian hedge- 30. Flurh JW, Mao-Qiang M, Brown BE, et al. Glycerol
hog and β-catenin signaling: role in the sebaceous regulates stratum corneum hydration in sebaceous
lineage of normal and neoplastic mammalian epi- gland deficient (Asebia) mice. J Invest Dermatol.
dermis. Proc Natl Acad Sci U S A. 2003;100(suppl 1): 2003;120:728-737.
11873-11880. 31. Zouboulis CC, Jourdan E, Picardo M. Acne is an inflam-
12. Allen M, Grachtchouk M, Sheng H, et al. Hedgehog matory disease and alterations of sebum composi-
signaling regulates sebaceous gland development. tion initiate acne lesions. J Eur Acad Dermatol Venereol. 85
Am J Pathol. 2003;163:2173-2178. 2014;28:527-532.
Kang_CH006_p0070-0088.indd 85 08/12/18 4:14 pm
2 32. Wille JJ, Kydonieus A. Palmitoleic acid isomer (C16:1d6) is
the active antimicrobial fatty acid in human skin sebum.
52. Zouboulis CC, Picardo M, Ju Q, et al. Beyond
acne: current aspects of sebaceous gland biology
Skin Pharmacol Appl Skin Physiol. 2003;16:176-187. and function. Rev Endocr Metab Disord. 2017;17:
33. Gebhart W, Metze D, Jurecka W. Identification of 319-334.
secretory immunoglobulin A in human sebaceous 53. Hong I, Lee MH, Na TY, et al. LXRα enhances lipid
and sweat glands. J Invest Dermatol. 1989;92:648. synthesis in SZ95 sebocytes. J Invest Dermatol. 2008;
34. Thiele JJ, Weber SU, Packer L. Sebaceous gland secre- 128:1266-1272.
tion is a major physiologic route of vitamin E delivery 54. Schmuth M, Watson RE, Deplewski D, et al. Nuclear hor-
to skin. J Invest Dermatol. 1999;113:1006-1010. mone receptors in human skin. Horm Metab Res. 2007;
35. Lee DY, Yamasaki K, Rudsil J, et al. Sebocytes express 39:96-105.
functional cathelicidin antimicrobial peptides and 55. Zouboulis CC. Sebaceous cells in monolayer culture.
can act to kill propionibacterium acnes. J Invest In Vitro Cell Dev Biol. 1992;28A:699.
Dermatol. 2008;128:1863-1866. 56. Zouboulis CC. Sebaceous gland in human skin—the
36. Lai Y, Gallo RL. AMPed up immunity: how antimicro- fantastic future of a skin appendage. J Invest Derma-
bial peptides have multiple roles in immune defense. tol. 2003;120:xiv-xv.
Trends Immunol. 2009;30:131-141. 57. Alestas T, Ganceviciene R, Fimmel S, et al. Enzymes
Part 2
37. Nakatsuji T, Kao MC, Zhang L, et al. Sebum free involved in the biosynthesis of leukotriene B4 and
fatty acids enhance the innate immune defense of prostaglandin E2 are active in sebaceous glands.
human sebocytes by upregulating beta-defensin-2 J Mol Med. 2006;84:75-87.
::
expression. J Invest Dermatol. 2010;130:985-984. 58. Imperato-McGinley J, Gautier T, Cai LQ, et al. The
38. Oeff MK, Seltmann H, Hiroi N, et al. Differential regu- androgen control of sebum production. Studies of
Structure and Function of Skin
lation of Toll-like receptor and CD14 pathways by subjects with dihydrotestosterone deficiency and
retinoids and corticosteroids in human sebocytes. complete androgen insensitivity. J Clin Endocrinol
Dermatology. 2006;213:266. Metab. 1993;76:524-528.
39. Lovászi M, Mattii M, Eyerich K, et al. Sebum lipids 59. Chen W, Tsai SJ, Sheu HM, et al. Testosterone syn-
influence macrophage polarization and activation. thesized in cultured human SZ95 sebocytes mainly
Br J Dermatol. 2017;177:1671-1682. derives from dehydroepiandrosterone. Exp Dermatol.
40. Mattii M, Lovászi M, Garzorz N, et al. Sebocytes con- 2010;19:470-472.
tribute to skin inflammation by promoting the dif- 60. Chen W, Thiboutot D, Zouboulis CC. Cutaneous
ferentiation of Th17 cells. Br J Dermatol. 2018;178(3): androgen metabolism: basic research and clinical
722-730. perspectives. J Invest Dermatol. 2002;119:992-1007.
41. Lovászi M, Szegedi A, Zouboulis CC, et al. Sebaceous 61. Fritsch M, Orfanos CE, Zouboulis CC. Sebocytes
immunobiology is orchestrated by sebum lipids. Der- are the key regulators of androgen homeostasis in
matoendocrinol. 2018;10:e1375636. human skin. J Invest Dermatol. 2001;116:793-800.
42. Zouboulis CC, Baron JM, Böhm M, et al. Frontiers 62. Azmahani A, Nakamura Y, Felizola SJ, et al. Steroido-
in sebaceous gland biology and pathology. Exp genic enzymes, their related transcription factors
Dermatol. 2008;17:542-551. and nuclear receptors in human sebaceous glands
43. Zouboulis CC, Adjaye J, Akamatsu H, et al. Human under normal and pathological conditions. J Steroid
skin stem cells and the ageing process. Exp Gerontol. Biochem Mol Biol. 2014;144B:268-279.
2008;43:986-997. 63. Zouboulis CC. Isotretinoin revisited—pluripotent
44. Fuchs E. Skin stem cells: rising to the surface. J Cell effects on human sebaceous gland cells. J Invest
Biol. 2008;180:273-284. Dermatol. 2006;126:2154-2156.
45. Serri F, Huber WM. The development of sebaceous 64. Ganceviciene R, Zouboulis CC. Isotretinoin for acne
glands in man. In: Montagna W, Ellis RA, Silver AF, eds. vulgaris: state-of-the-art treatment for acne vulgaris.
Advances in Biology of Skin. Vol. IV. Sebaceous Glands. J Dtsch Dermatol Ges. 2010;8(suppl 1):S47-S59.
Oxford: Pergamon; 1963:1-18. 65. Zouboulis CC, Korge B, Akamatsu H, et al. Effects of
46. Fenske NA, Lober CW. Structural and functional 13-cis-retinoic acid, all-trans-retinoic acid and acitre-
changes of normal aging skin. J Am Acad Dermatol. tin on the proliferation, lipid synthesis and keratin
1986;15:571-585. expression of cultured human sebocytes in vitro.
47. Zouboulis CC, Dessinioti C. Experimental models of J Invest Dermatol. 1991;96:792-797.
the sebaceous gland. In: Zouboulis CC, Katsambas 66. Tsukada M, Schröder M, Roos TC, et al. 13-cis Retinoic
AD, Kligman AM, eds. Pathogenesis and Treatment of acid exerts its specific activity on human sebocytes
Acne and Rosacea. Berlin: Springer; 2014:43-49. through selective intracellular isomerization to all-
48. Zouboulis CC, Xia L, Akamatsu H, et al. The human trans retinoic acid and binding to retinoid acid recep-
sebocyte culture model provides new insights into tors. J Invest Dermatol. 2000;115:321-327.
development and management of seborrhoea and 67. Hommel L, Geiger JM, Harms M, et al. Sebum excre-
acne. Dermatology. 1998;196:21-31. tion rate in subjects treated with oral all-trans-retinoic
49. Zouboulis CC, Schagen S, Alestas T. The sebocyte acid. Dermatology. 1996;193:127-130.
culture—a model to study the pathophysiology of 68. Mastrofrancesco A, Ottaviani M, Cardinali G, et al.
the sebaceous gland in sebostasis, seborrhoea and Pharmacological PPARγ modulation regulates sebo-
acne. Arch Dermatol Res. 2008;300:397-413. genesis and inflammation in SZ95 human sebocytes.
50. Schneider M, Zouboulis CC. Primary sebocytes and Biochem Pharmacol. 2017;138:96-106.
sebaceous gland cell lines for studying sebaceous 69. Trivedi NR, Cong Z, Nelson AM, et al. Peroxisome
lipogenesis and sebaceous gland diseases. Exp proliferator-activated receptors increase human
Dermatol. 2018;27(5):484-488. sebum production. J Invest Dermatol. 2006;126:
51. Nikolakis G, Stratakis CA, Kanaki T, et al. Skin 2002-2009.
86 steroidogenesis in health and disease. Rev Endocr 70. Zouboulis CC. Sebaceous gland receptors. Dermato-
Metab Disord. 2016;17:247-258. endocrinol. 2009;1:77-80.
Kang_CH006_p0070-0088.indd 86 08/12/18 4:14 pm
71. Russell LE, HarrisonWJ, Bahta AW, et al. Characterization
of liver X receptor expression and function in human
89. Nadel ER, Bullard RW, Stolwijk JA. Importance of skin
temperature in the regulation of sweating. J Appl
2
skin and the pilosebaceous unit. Exp Dermatol. 2007; Physiol. 1971;31(1):80-87.
16:844-852. 90. Freedman RR. Hot flashes: behavioral treatments,
72. Gross DN, van den Heuvel AP, Birnbaum MJ. The role mechanisms, and relation to sleep. Am J Med.
of FoxO in the regulation of metabolism. Oncogene. 2005;118(suppl 12B):124-130.
2008;27:2320-2336. 91. Johnson R, Spalding J. Disorders of the Autonomic Ner-
73. Dahlhoff M, Camera E, Picardo M, et al. PLIN2, the vous System. Philadelphia: FA Davis; 1974.
major perilipin regulated during sebocyte differenti- 92. Hu Y, Converse C, Lyons MC, et al. Neural control
ation, controls sebaceous lipid accumulation in vitro of sweat secretion: a review. Br J Dermatol. 2018;
and sebaceous gland size in vivo. Biochim Biophys 178(6):1246-1256.
Acta Gen Subjects. 2013;1830:4642-4649. 93. Kreyden OP, Scheidegger EP. Anatomy of the sweat
74. Camera E, Dahlhoff M, Ludovici M, et al. Perilipin 3 glands, pharmacology of botulinum toxin, and dis-
modulates specific lipogenic pathways in SZ95 sebo- tinctive syndromes associated with hyperhidrosis.
cytes. Exp Dermatol. 2014;23:759-761. Clin Dermatol. 2004;22(1):40-44.
75. Dahlhoff M, Camera E, Picardo M, et al. Angiopoietin- 94. Coon J, Rothman S. The sweat response to drugs with
Chapter 6 :: Skin Glands: Sebaceous, Eccrine, and Apocrine Glands
like 4, a protein strongly induced during sebocyte nicotine-like action. J Pharmacol Exp Ther. 1941;23:1.
differentiation, regulates sebaceous lipogenesis but 95. Faden AI, Chan P, Mendoza E. Progressive isolated seg-
is dispensable for sebaceous gland function in vivo. mental anhidrosis. Arch Neurol. 1982;39(3):172-175.
J Dermatol Sci. 2014;75:148-150. 96. Suzuki Y, Ohtsuyama M, Samman G, et al. Ionic basis
76. Borowczyk-Michalowska J, Zimolag E, Konieczny P, of methacholine-induced shrinkage of dissociated
et al. Stage-specific embryonic antigen-4 (SSEA-4) as a eccrine clear cells. J Membr Biol. 1991;123(1):33-41.
distinguishing marker between eccrine and apocrine 97. Buceta JM, Bradshaw CM, Szabadi E. Hyper-
origin of ducts of sweat glands. J Invest Dermatol. 2017; responsiveness of eccrine sweat glands to carbachol
137(11):2437-2440. in anxiety neurosis: comparison of male and female
77. Szabo G. The number of eccrine sweat glands in human patients. Br J Clin Pharmacol. 1985;19(6):817-822.
skin. In: Montagna W, Ellis R, Silver A, eds. Advances in 98. Sato K, Sato F. Defective beta adrenergic response of
Biology of Skin. New York: Pergamon; 1962:1. cystic fibrosis sweat glands in vivo and in vitro. J Clin
78. Sato K, Dobson RL. Regional and individual variations Invest. 1984;73(6):1763-1771.
in the function of the human eccrine sweat gland. 99. Prout BJ, Wardell WM. Sweating and peripheral blood
J Invest Dermatol. 1970;54(6):443-449. flow in patients with phaeochromocytoma. Clin Sci.
79. Schittek B, Hipfel R, Sauer B, et al. Dermcidin: a novel 1969;36(1):109-117.
human antibiotic peptide secreted by sweat glands. 100. Sato K. The physiology, pharmacology, and biochem-
Nat Immunol. 2001;2(12):1133-1137. istry of the eccrine sweat gland. Rev Physiol Biochem
80. Ali RS, Falconer A, Ikram M, et al. Expression of the Pharmacol. 1977;79:51-131.
peptide antibiotics human beta defensin-1 and 101. Sato K, Sato F. Na+, K+, H+, Cl−, and Ca2+ concentrations
human beta defensin-2 in normal human skin. J Invest in cystic fibrosis eccrine sweat in vivo and in vitro.
Dermatol. 2001;117(1):106-111. J Lab Clin Med. 1990;115(4):504-511.
81. Murakami M, Lopez-Garcia B, Braff M, et al. Postsecre- 102. Pagaduan JV, Ali M, Dowlin M, et al. Revisiting
tory processing generates multiple cathelicidins for sweat chloride test results based on recent guide-
enhanced topical antimicrobial defense. J Immunol. lines for diagnosis of cystic fibrosis. Pract Lab Med.
2004;172(5):3070-3077. 2018;10(1):34-37.
82. Hanukoglu I, Boggula VR, Vaknine H, et al. Expression 103. Sato K, Dobson RL. Glucose metabolism of the iso-
of epithelial sodium channel (ENaC) and CFTR in the lated eccrine sweat gland. II. The relation between
human epidermis and epidermal appendages. Histo- glucose metabolism and sodium transport. J Clin
chem Cell Biol. 2017;147(1):733-748. Invest. 1973;52(9):2166-2174.
83. Ellis R. Eccrine sweat glands: electron microscopy, 104. Brusilow SW, Gordes EH. The permeability of the
cytochemistry and anatomy. In: Jadassohn J, ed. sweat gland to nonelectrolytes. Am J Dis Child.
Handbuch der Haut und Geshlechtskrankheiten. Berlin: 1966;112(4):328-333.
Springer-Verlag; 1967:223. 105. Brusilow SW, Gordes EH. Ammonia secretion in
84. Sato F, Owen M, Matthes R, et al. Functional and mor- sweat. Am J Physiol. 1968;214(3):513-517.
phological changes in the eccrine sweat gland with 106. Page CO Jr, Remington JS. Immunologic studies in nor-
heat acclimation. J Appl Physiol. 1990;69(1):232-236. mal human sweat. J Lab Clin Med. 1967;69(4):634-650.
85. Saga K, Sato K. Ultrastructural localization of ouabain- 107. Jirka M, Blanicky P. Micro-isoelectric focusing of
sensitive, K-dependent p-nitrophenyl phosphatase proteins in pilocarpine-induced sweat. Clin Chim
activity in monkey eccrine sweat gland. J Histochem Acta. 1971;31(2):329-332.
Cytochem. 1988;36(8):1023-1030. 108. Yokozeki H, Hibino T, Takemura T, et al. Cysteine pro-
86. Sato K, Nishiyama A, Kobayashi M. Mechanical proper- teinase inhibitor in eccrine sweat is derived from
ties and functions of the myoepithelium in the eccrine sweat gland. Am J Physiol. 1991;260(2 Pt 2):R314-R320.
sweat gland. Am J Physiol. 1979;237(3):C177-C184. 109. Garden JW. Plasma and sweat histamine concentra-
87. Hashimoto K, Gross BG, Lever WF. The ultrastruc- tions after heat exposure and physical exercise. J Appl
ture of the skin of human embryos. I. The intraepi- Physiol. 1966;21(2):631-635.
dermal eccrine sweat duct. J Invest Dermatol. 1965; 110. Forstrom L, Goldyne ME, Winkelmann RK. Prostaglan-
45(3):139-151. din activity in human eccrine sweat. Prostaglandins.
88. Sato K, Dobson RL, Mali JW. Enzymatic basis for the 1974;7(6):459-464.
active transport of sodium in the eccrine sweat gland. 111. Seutter E, Sutorius AH. The vitamin K derivatives of
Localization and characterization of Na-K-adenosine some skin-mucins. 3. A route of oxygen transfer. Int 87
triphosphatase. J Invest Dermatol. 1971;57(1):10-16. J Vitam Nutr Res. 1971;41(4):529-536.
Kang_CH006_p0070-0088.indd 87 08/12/18 4:14 pm
2 112. Shah VP, Epstein WL, Riegelman S. Role of sweat in
accumulation of orally administered griseofulvin in
immunolocalization and functional demonstration.
Am J Physiol Cell Physiol. 2002;282(6):C1454-C1460.
skin. J Clin Invest. 1974;53(6):1673-1678. 124. Nejsum LN, Praetorius J, Nielsen S. NKCC1 and NHE1
113. Harris R, Jones HE, Artis WM. Orally administered are abundantly expressed in the basolateral plasma
ketoconazole: route of delivery to the human membrane of secretory coil cells in rat, mouse, and
stratum corneum. Antimicrob Agents Chemother. human sweat glands. Am J Physiol Cell Physiol. 2005;
1983;24(6):876-882. 289(2):C333-C340.
114. Vree TB, Muskens AT, van Rossum JM. Excretion of 125. de Carolis P, Magnifico F, Pierangeli G, et al. Tran-
amphetamines in human sweat. Arch Int Pharmaco- sient hypohidrosis induced by topiramate. Epilepsia.
dyn Ther. 1972;199(2):311-317. 2003;44(7):974-976.
115. Bolognia JL, Cooper DL, Glusac EJ. Toxic erythema of 126. Shappell SB, Keeney DS, Zhang J, et al.
chemotherapy: a useful clinical term. J Am Acad Der- 15-Lipoxygenase-2 expression in benign and neoplas-
matol. 2008;59(3):524-529. tic sebaceous glands and other cutaneous adnexa.
116. Sato K. The physiology and pharmacology of the J Invest Dermatol. 2001;117(1):36-43.
eccrine sweat gland. In: Goldsmith L, ed. Biochemistry 127. Charles A. An electron microscopic study of the human
and Physiology of the Skin. Oxford: Oxford University axillary apocrine gland. J Anat. 1959;93(2):226-232.
Part 2
Press; 1983:596. 128. Lindsay SL, Holmes S, Corbett AD, et al. Innerva-
117. Takemura T, Sato F, Saga K, et al. Intracellular ion tion and receptor profiles of the human apocrine
concentrations and cell volume during cholinergic (epitrichial) sweat gland: routes for intervention in
::
stimulation of eccrine secretory coil cells. J Membr bromhidrosis. Br J Dermatol. 2008;159(3):653-660.
Biol. 1991;119(3):211-219. 129. Mykytowycz R. The behavioural role of the mam-
Structure and Function of Skin
118. Reddy MM, Quinton PM. Cytosolic potassium con- malian skin glands. Naturwissenschaften. 1972;59(4):
trols CFTR deactivation in human sweat duct. Am 133-139.
J Physiol Cell Physiol. 2006;291(1):C122-C129. 130. Martin A, Saathoff M, Kuhn F, et al. A functional ABCC11
119. Sato K, Sato F. Cyclic AMP accumulation in the beta allele is essential in the biochemical formation of
adrenergic mechanism of eccrine sweat secretion. human axillary odor. J Invest Dermatol. 2010;130(2):
Pflugers Arch. 1981;390(1):49-53. 529-540.
120. Garty H, Palmer LG. Epithelial sodium channels: func- 131. Sato K. Pharmacological responsiveness of the myo-
tion, structure, and regulation. Physiol Rev. 1997; epithelium of the isolated human axillary apocrine
77(2):359-396. sweat gland. Br J Dermatol. 1980;103(3):235-243.
121. Granger D, Marsolais M, Burry J, et al. Na+/H+ exchang- 132. Wu JM, Mamelak AJ, Nussbaum R, et al. Botulinum
ers in the human eccrine sweat duct. Am J Physiol Cell toxin a in the treatment of chromhidrosis. Dermatol
Physiol. 2003;285(5):C1047-C1058. Surg. 2005;31(8 Pt 1):963-965.
122. Yamaga K, Murota H, Tamura A, et al. Claudin-3 loss 133. Robertshaw D. Apocrine sweat glands. In: Goldsmith L,
causes leakage of sweat from the sweat gland to ed. Physiology, Biochemistry and Molecular Biology of
contribute to the pathogenesis of atopic dermatitis. the Skin. Oxford: Oxford University Press; 1991:763.
J Invest Dermatol. 2018;138(6):1279-1287.
123. Granger D, Marsolais M, Burry J, et al. V-type
H+-ATPase in the human eccrine sweat duct:
88
Kang_CH006_p0070-0088.indd 88 08/12/18 4:14 pm
You might also like
- Human Histology 5.3 Glandular EpitheliumDocument6 pagesHuman Histology 5.3 Glandular EpitheliumBlubby BleuNo ratings yet
- Membranes & GlandsDocument7 pagesMembranes & GlandsabdulNo ratings yet
- Integumentary System 2Document7 pagesIntegumentary System 220237445No ratings yet
- Education Notes 2Document6 pagesEducation Notes 2Rwynn MemoryNo ratings yet
- Anaphy Mia Rev3Document5 pagesAnaphy Mia Rev3antonettevegamia3No ratings yet
- 4th Lecture On The Histology of Skin by Dr. RoomiDocument12 pages4th Lecture On The Histology of Skin by Dr. RoomiMudassar RoomiNo ratings yet
- Tissues, SkinDocument11 pagesTissues, SkinkimcheeseNo ratings yet
- NeoNotes Derma HighlightedDocument32 pagesNeoNotes Derma Highlightedyomna.saaNo ratings yet
- Vertebrate Integumentary System: By: Geonyzl J. Lepiten-AlviolaDocument93 pagesVertebrate Integumentary System: By: Geonyzl J. Lepiten-AlviolaGeonyzl L. AlviolaNo ratings yet
- Lec Activity4 Bdimayuga 10120Document5 pagesLec Activity4 Bdimayuga 1012002 - DIMAYUGA, BRYANNo ratings yet
- 2nd (Integumentary Activity)Document3 pages2nd (Integumentary Activity)Yma FeelNo ratings yet
- AnaPhyLec Midterms TissueDocument4 pagesAnaPhyLec Midterms TissueSoul YuNo ratings yet
- CH 7Document9 pagesCH 7Ruchika Kumari, VIII-A, 3956100% (1)
- Chapter-03 Structural Organisation in Animals: Animal TissueDocument5 pagesChapter-03 Structural Organisation in Animals: Animal TissueAravind Shabu100% (1)
- Chapter-03 Structural Organisation in Animals: Animal TissueDocument5 pagesChapter-03 Structural Organisation in Animals: Animal TissueAravind ShabuNo ratings yet
- Human TissuesDocument24 pagesHuman TissuesAna Doce MoralesNo ratings yet
- CH 7 Structural Organisation of AnimalsDocument16 pagesCH 7 Structural Organisation of AnimalsREENA GULERIANo ratings yet
- Kebo 107Document23 pagesKebo 107Manu MittalNo ratings yet
- Lab 04 Glandular EpitheliumDocument2 pagesLab 04 Glandular EpitheliumSarwar JafarNo ratings yet
- Epithelial Tissues 2024-01Document45 pagesEpithelial Tissues 2024-01jcrosa137No ratings yet
- Body TissuesDocument10 pagesBody TissuesAlther LorenNo ratings yet
- Cell StructureDocument8 pagesCell StructureCRYSTAL A. ARIETANo ratings yet
- 1.03 - Evidence of Science and Technology During The Ancient TimesDocument13 pages1.03 - Evidence of Science and Technology During The Ancient Timeselio pascualNo ratings yet
- T I S S U E: 4 Major Types of TissueDocument6 pagesT I S S U E: 4 Major Types of TissueMarla TurquezaNo ratings yet
- ch-7 Bio Grade 11Document18 pagesch-7 Bio Grade 11shurshtikarande18No ratings yet
- Exercise 1: Epithelial TissueDocument6 pagesExercise 1: Epithelial TissueTherese RiveraNo ratings yet
- A&P1 Final Exam Study GuideDocument7 pagesA&P1 Final Exam Study GuideRhett ClarkNo ratings yet
- DelaCruz AlbertBryan Activity#6 MED3Document2 pagesDelaCruz AlbertBryan Activity#6 MED3AlbertNo ratings yet
- 7 Structural Organisation in Animals - Notes - SampleDocument2 pages7 Structural Organisation in Animals - Notes - SampleManish KumarNo ratings yet
- TissueDocument7 pagesTissueGodhuli SahooNo ratings yet
- Report Glandular EpitheliumDocument11 pagesReport Glandular EpitheliumKang MonNo ratings yet
- JI UNIT 2 Complete Notes - 11-12Document2 pagesJI UNIT 2 Complete Notes - 11-12Shubham PawadeNo ratings yet
- Chapter 4 TissuesDocument9 pagesChapter 4 TissuesBaylon, MarkNo ratings yet
- Glandular Epithelium: Descriptive HistologyDocument23 pagesGlandular Epithelium: Descriptive HistologyIan LubangaNo ratings yet
- Body TissuesDocument10 pagesBody TissuesAlther LorenNo ratings yet
- TissueDocument22 pagesTissueRuhul Qudus NaimNo ratings yet
- MT1 HSCI LEC L3 Integumentary SystemDocument9 pagesMT1 HSCI LEC L3 Integumentary SystemSEBASTIEN ANDREI BUENAFENo ratings yet
- Chapter Four: YANES, Myngelle C. Anaphy Bmls 02Document4 pagesChapter Four: YANES, Myngelle C. Anaphy Bmls 02cheewyyyyNo ratings yet
- B 28-MIBS-Histology Log Book - Model DiagramDocument27 pagesB 28-MIBS-Histology Log Book - Model DiagramSANTHIYA A/P MOHANA SUNDARAM MoeNo ratings yet
- Tob 2.2Document29 pagesTob 2.2LT DRAGONXNo ratings yet
- Epithelial Tissue (Epithelium) : General Characteristics of EpitheliumDocument22 pagesEpithelial Tissue (Epithelium) : General Characteristics of EpitheliumMahmoud IdlbiNo ratings yet
- Anaphy ReviewerDocument32 pagesAnaphy Reviewerpatientsafety100% (1)
- Integumentary System: 1. Mouth/ ProstomiumDocument4 pagesIntegumentary System: 1. Mouth/ ProstomiumMark Robert Magsino100% (1)
- Animal TissuesDocument75 pagesAnimal TissuesFaithlyn Riche YocorNo ratings yet
- Chapter 6:: Skin Glands: Sebaceous, Eccrine, and Apocrine GlandsDocument32 pagesChapter 6:: Skin Glands: Sebaceous, Eccrine, and Apocrine GlandsS FznsNo ratings yet
- WEEK 4 TissuesDocument15 pagesWEEK 4 TissuesMarjorie Lyka LingatNo ratings yet
- Animal Histology Notes - EpiitheliumDocument10 pagesAnimal Histology Notes - Epiitheliumsy8No ratings yet
- ملخص اناتومي مهم مليونDocument7 pagesملخص اناتومي مهم مليونSaif AltamareNo ratings yet
- 2.medical School Histology Epithelium and GlandsDocument50 pages2.medical School Histology Epithelium and GlandsPhaniNo ratings yet
- Lab 5 Tissues - Lab ReportDocument5 pagesLab 5 Tissues - Lab ReportbrittNo ratings yet
- Anaphy ReviewerDocument13 pagesAnaphy ReviewerChriza Mae Dela Pe�aNo ratings yet
- Kebo107 PDFDocument23 pagesKebo107 PDFbashraaNo ratings yet
- L2.2 - Inner - Surfaces 5thmarch, 2022Document31 pagesL2.2 - Inner - Surfaces 5thmarch, 2022TalarNo ratings yet
- HistologyDocument16 pagesHistologyJeong song parkNo ratings yet
- Anaphy - Tissue - Part 1Document5 pagesAnaphy - Tissue - Part 1Aileen DemaguilaNo ratings yet
- Chapter 2 CytogeneticsDocument13 pagesChapter 2 CytogeneticsKathleen TanateNo ratings yet
- Cell 4Document80 pagesCell 4jocajoldinNo ratings yet
- Animal Tissue & Organ System: SMA Pradita DirgantaraDocument30 pagesAnimal Tissue & Organ System: SMA Pradita Dirgantarahafiz amriNo ratings yet
- Test Bank For Accompany Saladin Human Anatomy 6th Edition Eric Wise DownloadDocument35 pagesTest Bank For Accompany Saladin Human Anatomy 6th Edition Eric Wise Downloadstevenmccallcdrjybmage100% (23)
- Dermatology - James G. Marks, Jeffrey J. Miller - Lookingbill and Marks' Principles of Dermatology (2018, Elsevier) (Dragged)Document9 pagesDermatology - James G. Marks, Jeffrey J. Miller - Lookingbill and Marks' Principles of Dermatology (2018, Elsevier) (Dragged)nh2411No ratings yet
- Physiology of INTEGUMENTARY SYSTEM FK PDFDocument84 pagesPhysiology of INTEGUMENTARY SYSTEM FK PDFdaris agharidNo ratings yet
- Anatomical and Physiological Differences Between Child and AdultDocument8 pagesAnatomical and Physiological Differences Between Child and AdultNeethu Mohandas86% (7)
- Unit VI Lecture NotesDocument5 pagesUnit VI Lecture NotesSteve Sullivan100% (1)
- Integumentary System - NUR1019 - 20sept2022Document33 pagesIntegumentary System - NUR1019 - 20sept2022琪琪No ratings yet
- 101-Normal Skin MCQsDocument25 pages101-Normal Skin MCQsHybat ElsheikhNo ratings yet
- Skin Nail HairDocument48 pagesSkin Nail HairkitsilcNo ratings yet
- AP 5 Integumentary SystemDocument120 pagesAP 5 Integumentary SystemIkhsan HidayatNo ratings yet
- Glandular EpitheliumDocument34 pagesGlandular EpitheliumAnonymous WBMLOgPNo ratings yet
- Basic Science and Sructure of Skin MCQsDocument92 pagesBasic Science and Sructure of Skin MCQsDr.Tawheed88% (17)
- Histology MCQs Part 2Document54 pagesHistology MCQs Part 2RPh Krishna Chandra Jagrit71% (7)
- Science 6 TG q2Document112 pagesScience 6 TG q2Pinaka ShungaNo ratings yet
- Veterinary Clinical Diagnosis DVM 2022-23Document51 pagesVeterinary Clinical Diagnosis DVM 2022-23MilkiyasNo ratings yet
- Body Malodours and Their Topical Treatment AgentsDocument14 pagesBody Malodours and Their Topical Treatment AgentsChiper Zaharia DanielaNo ratings yet
- Anatomy of SkinDocument25 pagesAnatomy of Skinaimi Batrisyia100% (1)
- Robbery EssayDocument4 pagesRobbery Essayafhexydml100% (2)
- Azza Mohamed Ahmed Said Professor of Ophthalmology Ain Shams UniversityDocument54 pagesAzza Mohamed Ahmed Said Professor of Ophthalmology Ain Shams UniversityraeNo ratings yet
- What Is The Source of FingerprintDocument68 pagesWhat Is The Source of FingerprintAvy GuisadoNo ratings yet
- Integumentary SystemDocument24 pagesIntegumentary SystemGJ Badenas100% (1)
- Structure of SkinDocument129 pagesStructure of SkinDeepak BaliyanNo ratings yet
- Lect Skin4aDocument98 pagesLect Skin4akazchandranNo ratings yet
- Chapter 5 Integumentary SystemDocument89 pagesChapter 5 Integumentary SystemCal GoNo ratings yet
- Nursing in Dermatovenereology. 1Document66 pagesNursing in Dermatovenereology. 1aboadam889122No ratings yet
- Zoology Notes: 009 Chapter 5Document4 pagesZoology Notes: 009 Chapter 5humanupgrade100% (1)
- Development of Integumentary Sytem With AudioDocument36 pagesDevelopment of Integumentary Sytem With AudioRetrocasualty Find OutNo ratings yet
- Lab Worksheet No. 5 Integumentary SystemDocument15 pagesLab Worksheet No. 5 Integumentary SystemKarylle Ezra GulifardoNo ratings yet
- 978 0323049092 Color Textbook of Pediatric Dermatology Color Textbook of Pediatric Dermatology WestonDocument61 pages978 0323049092 Color Textbook of Pediatric Dermatology Color Textbook of Pediatric Dermatology Westonaudrey.walston606100% (42)
- Clinical Ophthalmic Oncology Eyelid and Conjunctival TumorsDocument239 pagesClinical Ophthalmic Oncology Eyelid and Conjunctival TumorsRosa SoledadNo ratings yet
- ch08 Integumentary System The Protective CoveringDocument96 pagesch08 Integumentary System The Protective CoveringRYAN JAY PASTORNo ratings yet